Case Presentation:
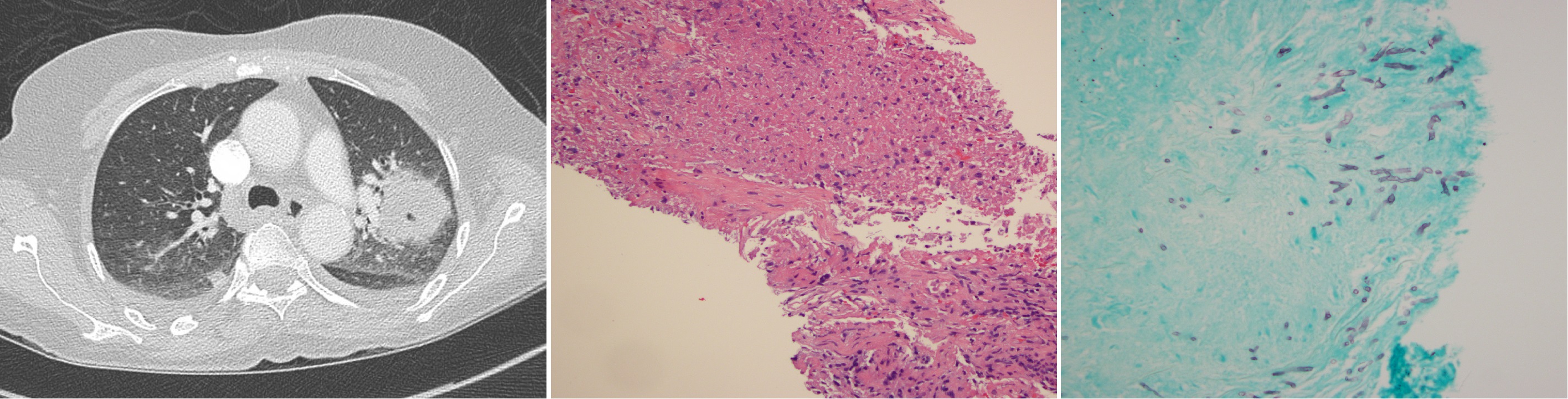
A 60 year-old Polish woman with stage IV adenocarcinoma of the lung (ALK fusion oncogene positive) on crizotinib, with a recent history of steroid use, presented with one week of malaise. In the Emergency Department she was febrile to 101.3 °F. A chest x-ray demonstrated a left lobar infiltrate. The patient was started on ceftriaxone and azithromycin, and admitted for presumed community-acquired pneumonia. On hospital day three recurrent fever prompted a chest CAT scan showing progression of malignancy, as well as a new cavitary lesion corresponding to the abnormality seen on x-ray. An admission sputum culture grew Aspergillus fumigatus and voriconazole was started. Serum testing for (1,3)-Beta-D-Glucan was markedly elevated (>500 pg/mL) but was negative for Aspergillus Galactomannan antigen. The patient underwent percutaneous biopsy of the left upper lobe lesion and resulting cultures grew Aspergillus fumigatus. The patient remained afebrile and was discharged home on voriconazole and ciritinib.
Discussion:
ALK mutation is rare in non-small cell lung cancer (4% of patients), and occurs independently of KRAS and EGFR mutations. Crizotinib is a first generation ALK tyrosine kinase inhibitor approved for treatment of metastatic ALK positive disease. Neutropenia, and pneumonitis are well documented complications of therapy. Ceritinib, a more potent ALK inhibitor, can be used when tumors inevitably develop resistance to crizotinib via structural changes including the L1196M “gatekeeper” mutation. A third ALK inhibitor alectinib is currently under development.
Aspergillus conidia frequently enter the lower respiratory tract and are cleared by alveolar macrophages. In the presence of immunosuppression, conidia can germinate into hyphae with invasion into tissue opposed by neutrophil recruitment and activation. Major risk factors for development of invasive aspergillosis include severe or prolonged neutropenia, high dose glucocorticoid use, and impairment of cellular immunity. Tuberculosis, bronchiectasis, and cystic fibrosis also predispose to colonization because of abnormal clearance mechanisms. However, cavitary lesions caused by NSCLC are rarely associated with aspergillosis with only two documented case reports. Though crizotinib is known to cause neutropenia and is associated with upper respiratory tract infections, a review of the original data suggests that pulmonary complications are rare, with only 2% developing pneumonitis and less than 1% developing pneumonia.
Conclusions:
ALK inhibitors like crizotinib have become the standard of care for a small population of patients with NSCLC. An important side effect of these medications is neutropenia. Though pulmonary complications are rare they include pneumonitis and pneumonia. We present a patient with invasive pulmonary aspergillosis secondary to steroid use and cavitary NSCLC and postulate that crizotinib may have contributed.