Background:
Many patients who are admitted to the hospital might get resuscitated against their wishes, or their wishes might never be known if a discussion on code status has not been held. Patients get admitted to the hospital when they are the sickest, and hence sensitive communication at the time of admission is necessary in order to avoid resuscitation against wishes. Patient Self Determination Act (PSDA) requires that all patients be asked about their care wishes at the time of admission and document the presence of an advanced directive and code status. Code Status is a term used to describe the desire for resuscitation if needed and is performed as per Advanced Cardiac Life Support (ACLS) guidelines.
Methods:
A quality initiative project was conducted at the Robert Packer Hospital from November 1st until November 25th, 2014. All patients admitted by the medical residents on floor and ICU were included. Review of order entry in electronic medical record and charts for code status was assessed for data gathering. Various interventions including educating residents, displaying pamphlets in the admitting rooms for residents, educating nursing staffs to remind the residents and sending electronic reminders to the residents were done. Pre and post intervention data was gathered. At the end of pre-intervention period, a survey was done amongst all the residents to find out major reasons for not addressing code status.
Results:
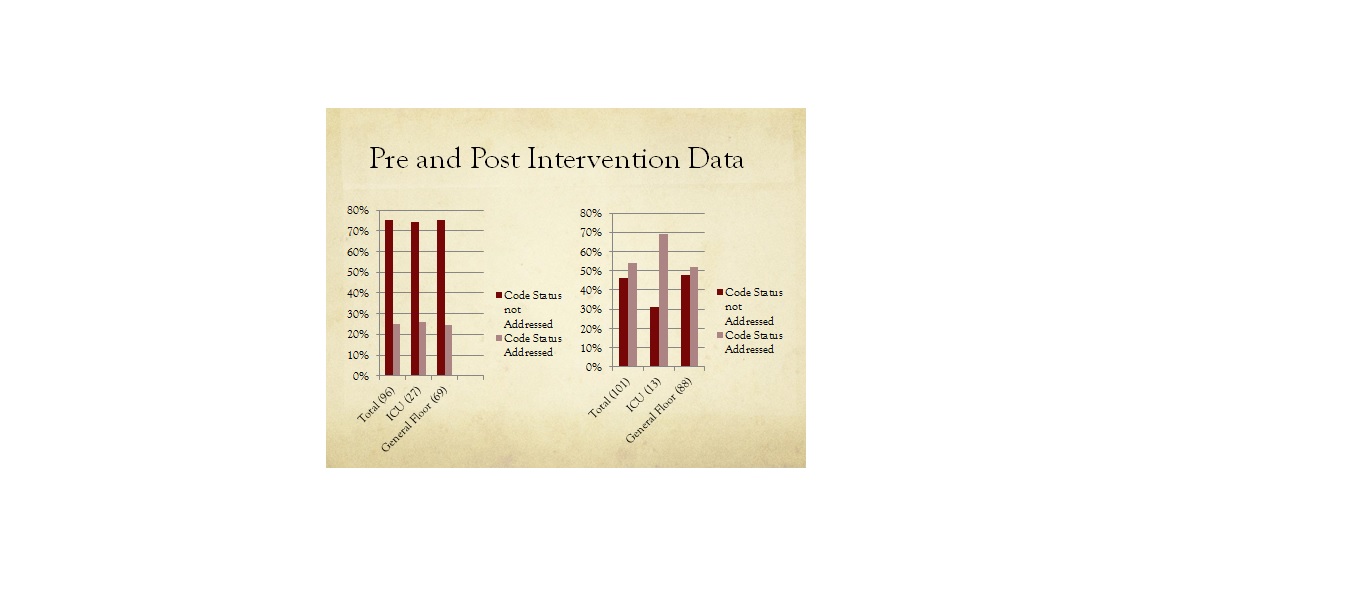
A total of 96 patients were in the pre-intervention group and 101 patients in the post-intervention group. Pre-intervention, code status was addressed in 25% of total admissions, 25.92% of ICU admissions and 24.63% of floor admissions. Post intervention, addressing of code status significantly increased to 54.45% of total admissions, 69.23% of ICU admissions and 52.27% of floor admissions. Survey showed that most of the residents do not address the code status when it is felt that the patients are not too sick (46.42%), time limitations (28.43%), patient too young (14.28%) and not enough rapport with the patient (10.71%).
Conclusions:
This project was undertaken to increase the awareness on a crucial aspect of the admission process i.e. addressing code status. Post intervention study showed that the rate of addressing code status significantly increased however there is still a gap between actual practice and PSDA requirement. In order to fill the gap, we propose that addressing code status be a mandatory process or a reminder be generated in electronic health records. Also, education of residents must be an ongoing process. This will help minimize unnecessary resuscitation leading to cost effective care and will help respect patient’s wishes.