Background: Transportation is a social determinant of health that can be a barrier to care and exacerbate disparities. During the COVID pandemic, access to transport was further diminished.Monoclonal antibodies (Mab) are associated decreased hospitalization in high-risk COVID patients. Until 9/2022, the $2000 cost per dose of Mabs was paid by the federal government. However transportation of COVID positive patients to an infusion site was not included in the federal program.The Mab infusion center operated by Baltimore Convention Center Field Hospital (BCCFH) provided free transportation to patients. We analyze the use of this service by vulnerable populations.
Methods: Patients receiving Mab infusion at BCCFH between 1/6/2021 and 5/31/2021 were included. BCCFH is a partnership between Maryland Department of Health and two academic medical centers. BCCFH started as a COVID overflow inpatient service in the convention center in Baltimore city. Because of lack of ambulatory space in existing health system to accommodate COVID patients, the BCCFH inpatient team created space and capabilities to provide Mab infusions. Treatment was provided with no out-of-pocket payment irrespective of insurance status. All patients were offered free, state-funded transportation using a Covid-safety compliant car service. Univariate logistic regression was used to assess the association between BCCFH transport use and demographic characteristics, including poverty zip code level data from census dataset. Poverty level in zip code of residence was categorized as low (0-10%), moderate (10-20%) and high (>20%). Referral-to-treatment time was compared between transport users and non-users. Cost of transportation was summarized.
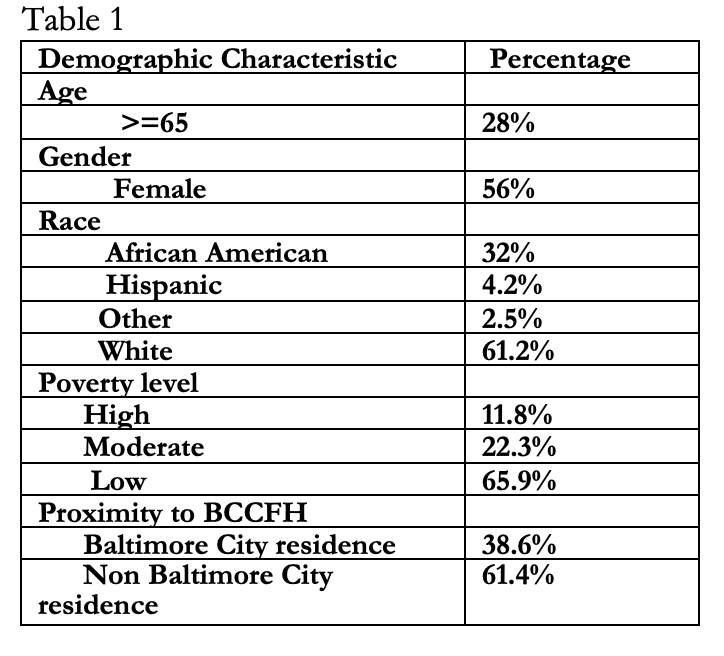
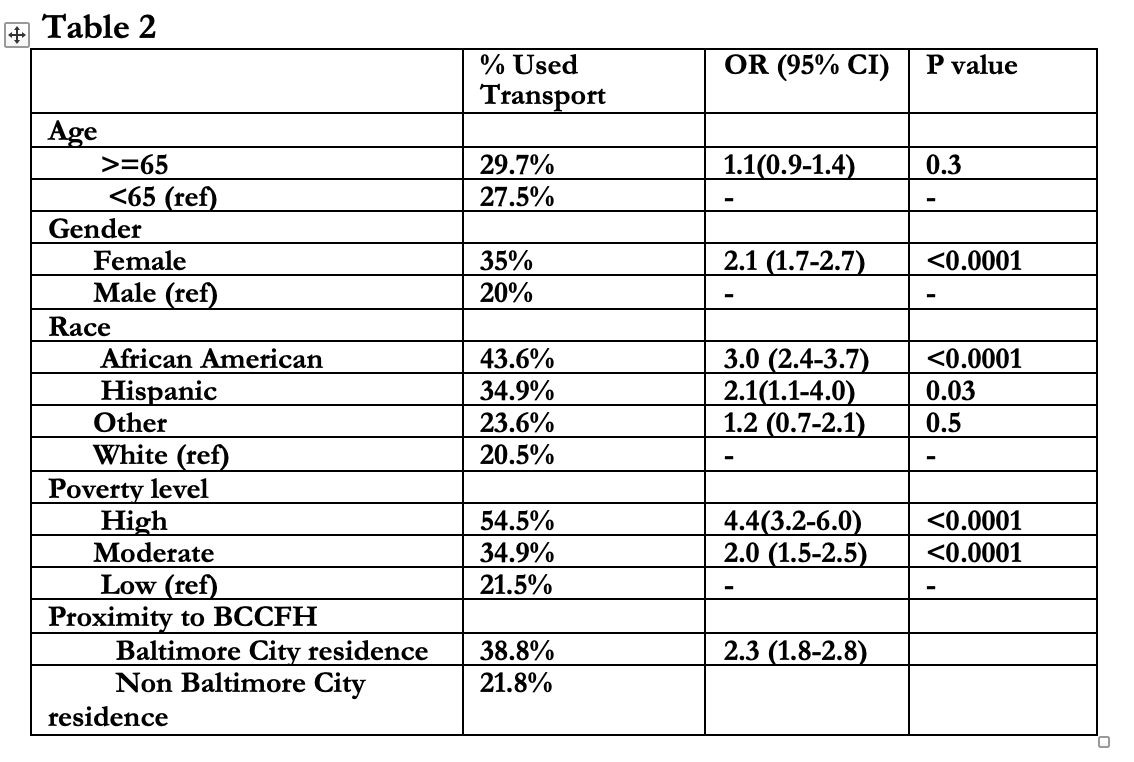
Results: 1708 were patients treated at BCCFH during this period, of which 61.3% were white, 28% were at or greater that 65 years of age, 56% were female and 11.8% were from high poverty zip codes (Table 1). 28.3% patients used transportation. Patients using transportation were more likely to be local city residents (OR 2.3 95% CI 1.8-2.8), female (OR 2.1 95% CI 1.7-2.7), African American (OR 3.0 95% CI 2.4-3.7), Hispanic ( OR 2.1 95% CI 1.1-4.0), and from a high poverty zip code ( OR 4.4 95% CI 3.2-6.0) (Table 2). African American patients from high poverty zip codes had 6.7 (95% CL: 4.6-9.6) times the odds of using BCCFH transport as white patients from low poverty zip codes. Transport users had a slightly longer interval between referral and appointment [1.6 (95% CI 1.5-1.7) days vs. 1.8 (95% CI 1.7-1.9) days P=0.005). The mean cost of the trip was $153 per patient transported and $43 per patient treated at BCCFH.
Conclusions: Even though monoclonal antibody treatment was sought mostly by Whites (61.2%) and those from wealthier neighborhoods (65.9%), free transportation was more likely used by vulnerable groups such as female, racial minorities and impoverished individuals. There were no clinically insignificant delays (0.2 days) for transport users from the time of referral. Local city resident disproportionately used transportation compared to those outside the city, suggesting that transportation use was not driven by convenience for those with longer commute. The $43 cost per patient treated was around only 2% of the $2000 cost for a dose of Mab paid by the federal government. Future federal pandemic programs should consider providing additional resources like transportation to reduce disparities and prevent hospitalizations.