Background:
Patients hospitalized for acute exacerbations of chronic obstructive pulmonary disease (AECOPD) are at high risk for readmission. In September 2012, a COPD longitudinal inpatient pathway and transition (CLIPT) was implemented at a 552-bed academic tertiary care medical center, created by a collaboration of hospitalists, pulmonologists, respiratory therapists, pharmacists and information systems specialists. We demonstrated previously that CLIPT improved adherence to international guidelines but did not significantly reduce readmission rates.
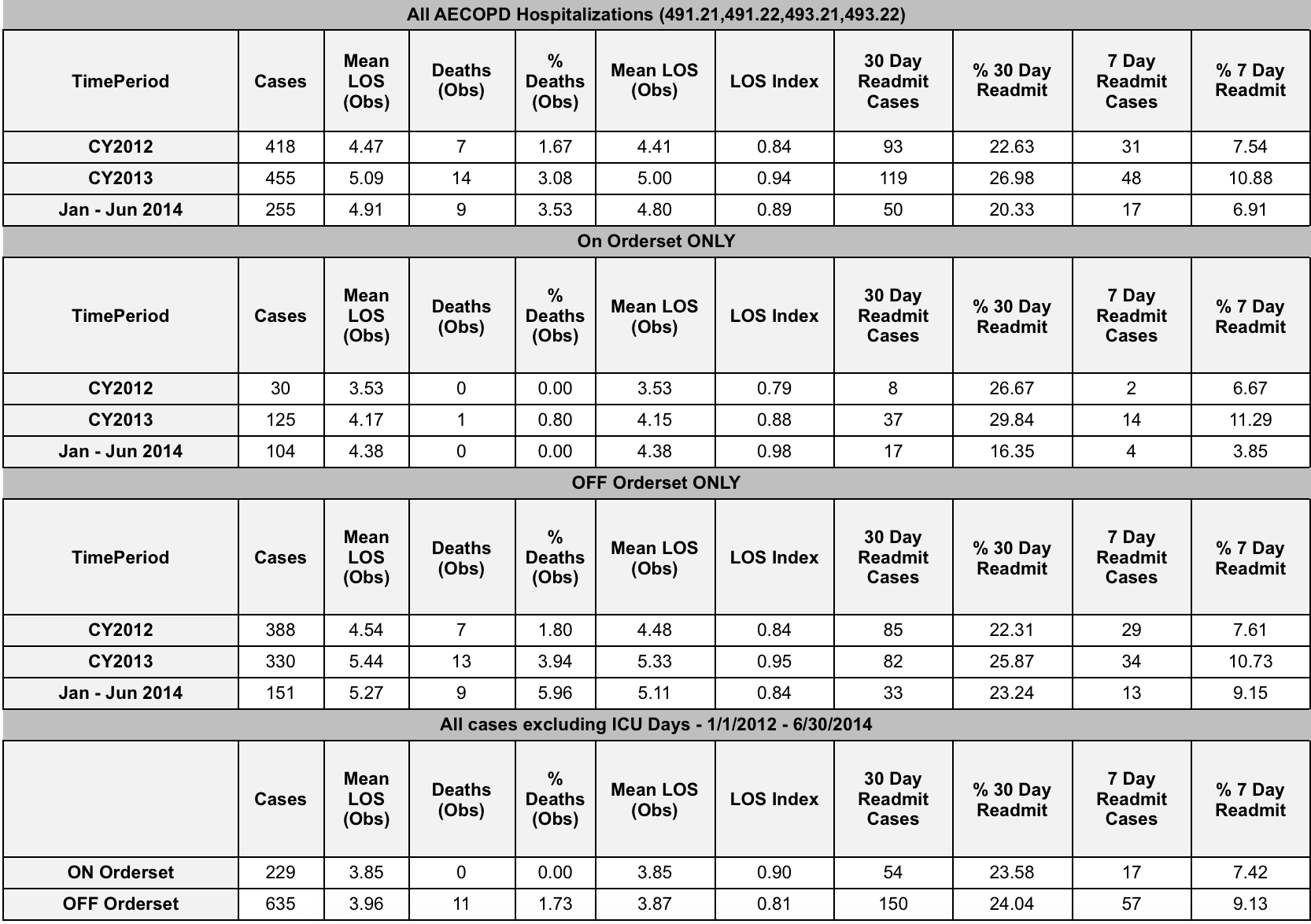
Methods: After instituting the initial computerized order entry clinical pathway that standardized pharmacologic therapies, respiratory care interventions and ancillary services, a multidisciplinary group instituted further enhancements based on QI methodology. These including improvements in pathway penetration, AECOPD identification and linkages to a newly-established airway clinic established in November 2013. We analyzed subsequent outcomes, including 7- and 30-day readmission rates, length of stay and mortality using risk-adjusted data from the University HealthSystem Consortium (UHC) database. Hospitalizations that included time in ICU were excluded in a subanalysis. AECOPD hospitalizations were identified by using ICD-9 billing codes.
Results: Over a 30-month period, 864 AECOPD non-ICU hospitalizations were identified. Overall, inpatient order sets were used in 27% of AECOPD hospitalizations but rose to 41% in the last 6 months. Order set usage was associated with slightly shorter length of stay (3.85 days vs. 3.96 days), lower 7-day readmission rate (7.4% vs. 9.1%), but similar 30-day readmission rate (23.6% vs 24.0%). Mortality was lower with order set usage (0% vs 1.73%). Airway clinic utilization since its inception in November 2013 was low with a 16% referral rate after AECOPD hospitalization and a subsequent 20% successful attendance rate. The 30-day readmission rate for patients who successfully attended the clinic during the study period was 5.7%
Conclusions: Implementation of CLIPT was associated with small reductions in length of stay, 7-day readmission rate, and mortality, although 30-day readmission rate was unchanged. Utilization of the order set and successful referral to the post-discharge clinic was low, but the latter was associated with a reduction in 30-day readmission rates. To address these shortcomings and further improve pathway penetration and transitions of care, a pilot program of a respiratory therapist COPD coordinator is planned to improve adherence to CLIPT, communication between inpatient and outpatient providers, and patient-centered education.