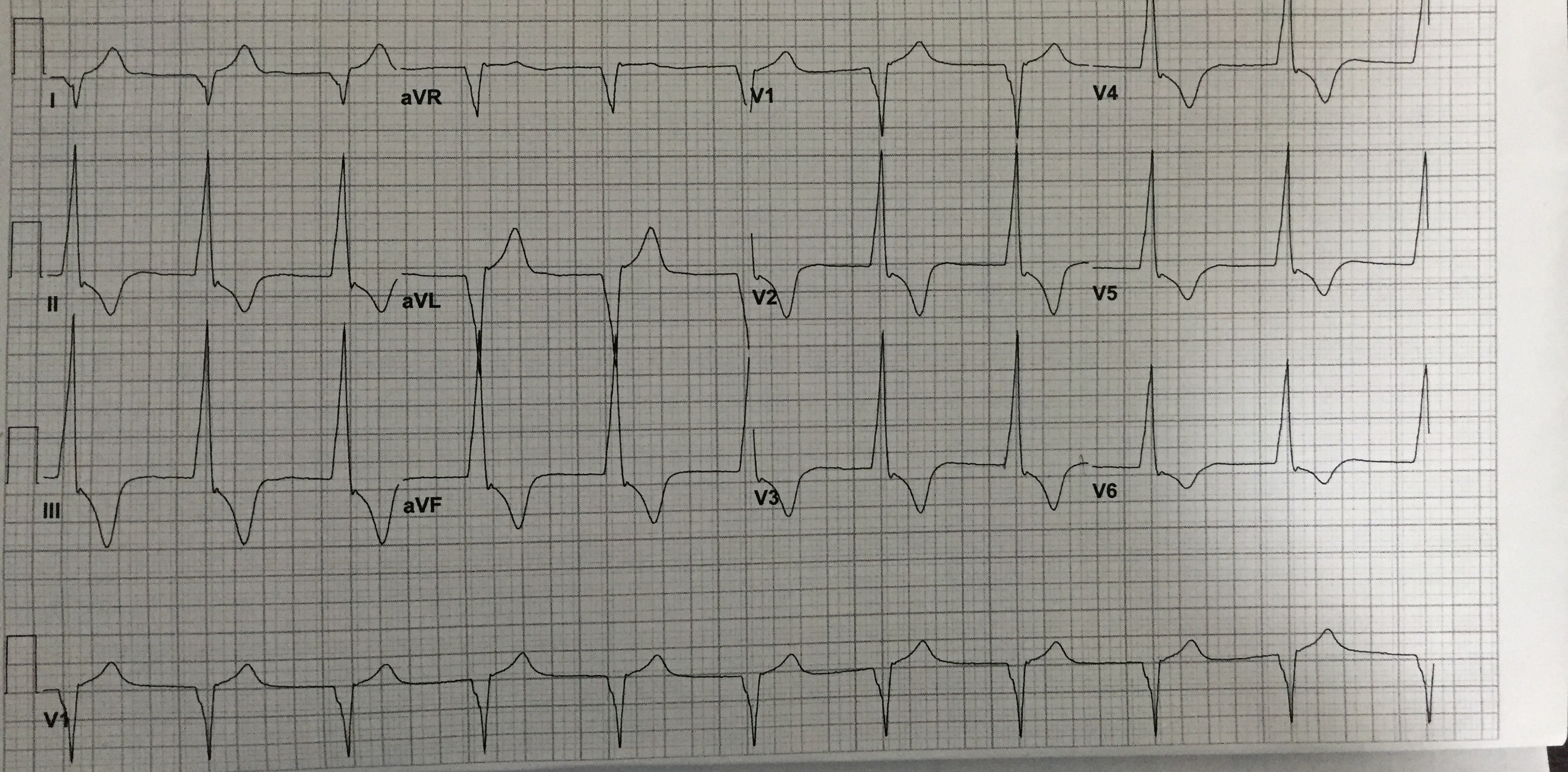
Case Presentation: We discuss here a 39-year-old female who presented to the emergency department after an unwitnessed fall followed by loss of consciousness due to alcohol intoxication. The physical examination was unremarkable except for a laceration over her scalp. She denied chest pain, shortness of breath, seizures, palpitations or dizziness. She had no history of coronary artery disease or previous syncope. CT head without contrast revealed a subarachnoid hemorrhage involving the right frontal, temporal and parietal lobes with a minimal leftward midline shift. She was conservatively monitored in the intensive care unit for one day. The next day, she developed asymptomatic bradycardia and her electrocardiogram showed a junctional rhythm with a wide QRS complex, prolonged QTc (>500ms), tall R waves, and T wave inversions. Electrolyte parameters, blood counts, TSH and troponin levels were normal. Echocardiogram was normal except for mild tricuspid regurgitation. The patient was hemodynamically stable and a repeat EKG the following morning was normal except for sinus bradycardia.
Discussion: EKG changes occur in 50% patients with SAH. These changes typically include tall R waves, ST depression, deeply inverted T waves and a prolonged QT interval, can appear up to 48 hours after SAH. Catecholamines, released in massive quantities due to hypothalamic stress from subarachnoid haemorrhage, result in acute, reversible cardiac injury ranging from hypokinesis with a normal cardiac index, to low output cardiac failure. This neurogenic stunned myocardium produces arrhythmias and accompanying EKG changes. Major predictive factors for mortality in patients presenting with SAH and EKG changes were an increase in serum troponin and T wave changes. The presence of intraventricular blood has been associated with a higher incidence of ventricular arrhythmias, particularly in patients with a prolonged QTc interval, which can often lead to hemodynamic compromise. The EKG changes resolve once SAH clears up so continuous monitoring and regulation of electrolytes is of utmost importance.
Conclusions: SAH is associated with certain EKG changes like bradycardia due to Cushing’s reflex, QT prolongation and giant T wave inversions called cerebral T waves. Improved outcomes can be seen by preventing further autonomic stress, giving beta blockers and avoiding drugs that prolong ventricular repolarization.