Background: Delirium, a highly morbid condition affecting significant numbers of hospitalized adults, is under-recognized due to challenges in monitoring patients’ waxing and waning symptoms. In addition, precipitating environmental factors such as light, sound, and sleep are difficult to observe. Computer vision cameras that can generate continuous observations of patients and their in-room care environment have the potential to monitor the risk factors and symptoms of delirium. However, the feasibility of this approach in real-world hospital settings is unclear.
Purpose: To assess the feasibility and clinical utility of an artificial intelligence-powered computer vision camera to monitor patients at high risk of delirium.
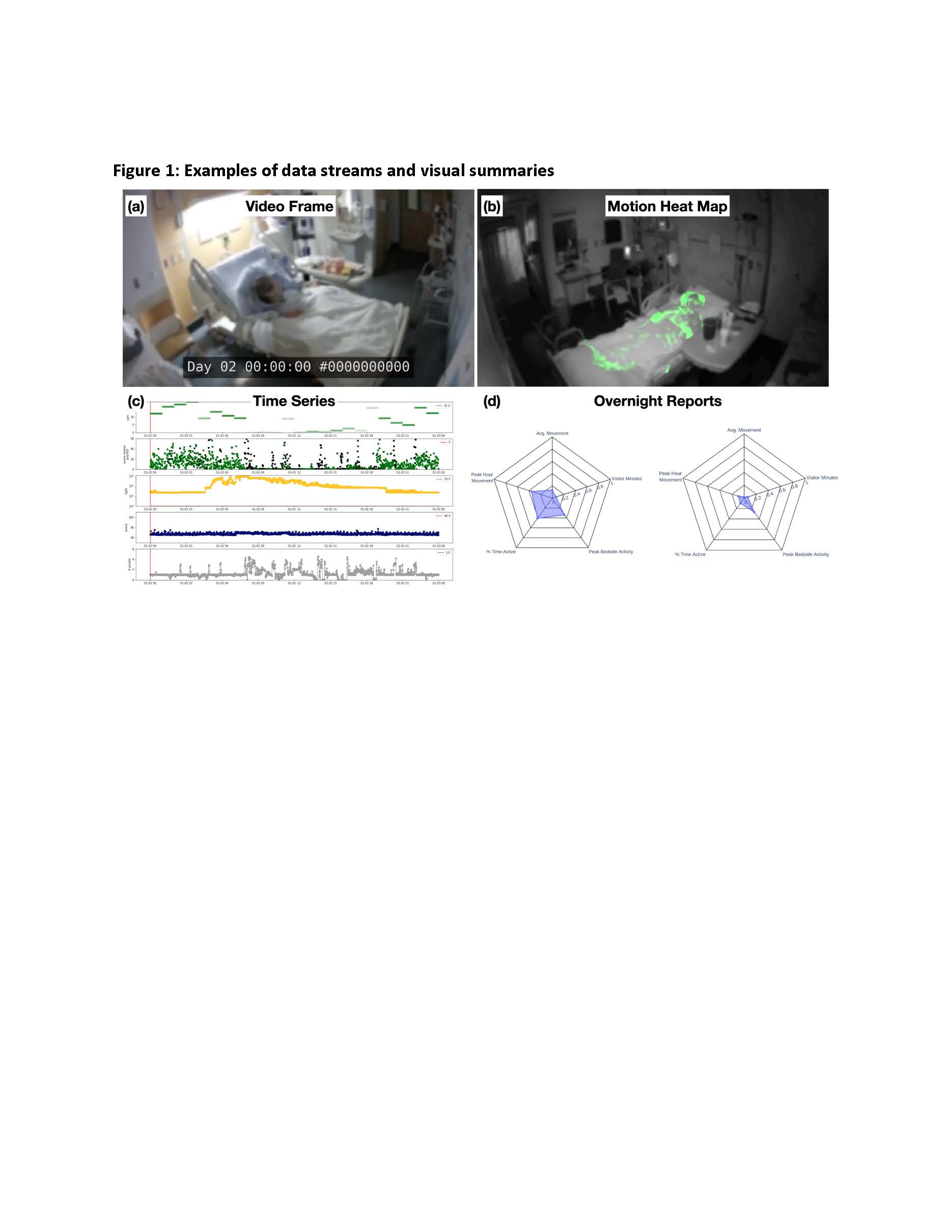
Description: This feasibility study was conducted on an Acute Care for Elders (ACE) unit at a quaternary care academic medical center between May 2021 and February 2022. A computer vision cart was deployed to consenting patient’s room for continuous video monitoring and data acquisition. The computer vision cart had a color and night vision cameras as well as light- and sound-level sensors. Data was streamed from the cameras and sensors to an encrypted hard drive on the cart. Data captured are interpreted to produce color images of daytime and nighttime activity, sleep nighttime wakefulness, agitation, prolonged somnolence, and staff bedside activity. Data about the room environment (i.e., light and sound levels) were collected that quantified high ambient light levels during the night but also light “pollution” from screens in the room. In total, data from 44 hospital days (744 hours) were captured and no patients were identified as delirious as measured by a delirium screening tool. Artificial intelligence algorithms analyzed video data to create a series of de-identified video data streams (Fig 1a) and visual summaries (Fig 1b) of patient activity and environmental factors that can be accessed by the clinical care team including patient movement and bedside activity, light, sounds and wakefulness. These summaries could be visualized at a minute-to-hour time level for each data element captured (Fig 1c). A graphic overnight report (Fig 1f) was created that provides a snapshot of five key dimensions and risk factors for delirium to inform clinical care.
Conclusions: We demonstrated the initial feasibility of artificial intelligence-powered computer vision camera to capture key elements of patient activity and environmental factors that may contribute to the risk of delirium. Next steps include correlation between these captured activity, sleep, and environmental levels and the incidence and prevalence of delirium.