Case Presentation: A previously healthy 26-year-old Caucasian man presented with 2 weeks of upper extremity edema in the setting of 4 months of productive cough with blood-tinged sputum, arthralgias, unintentional weight loss, and fatigue. On presentation, he was afebrile, tachycardic, and hypertensive with stable oxygen saturation. Laboratory data was notable for hemoglobin of 5.5 g/dL, 16,500 white blood cells/μL and creatinine of 1.9 mg/dL. Shortly after admission, the patient experienced massive hemoptysis with bedside bronchoscopy revealing severe diffuse alveolar hemorrhage (DAH). He was emergently intubated and treated empirically for presumed vasculitis with high dose steroids. Despite this, DAH persisted and resulted in severe acute respiratory distress syndrome requiring extracorporeal membrane oxygenation (ECMO).
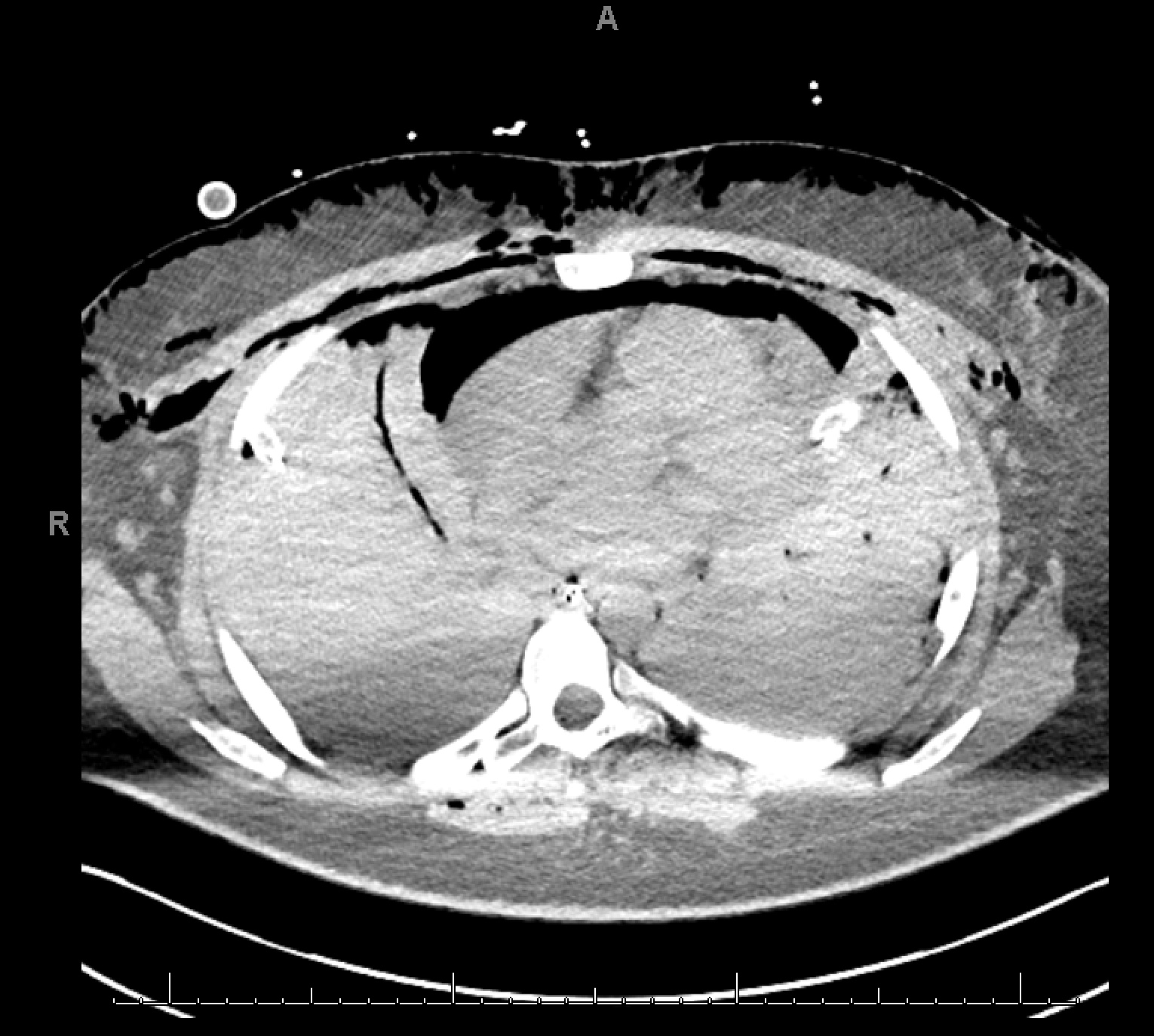
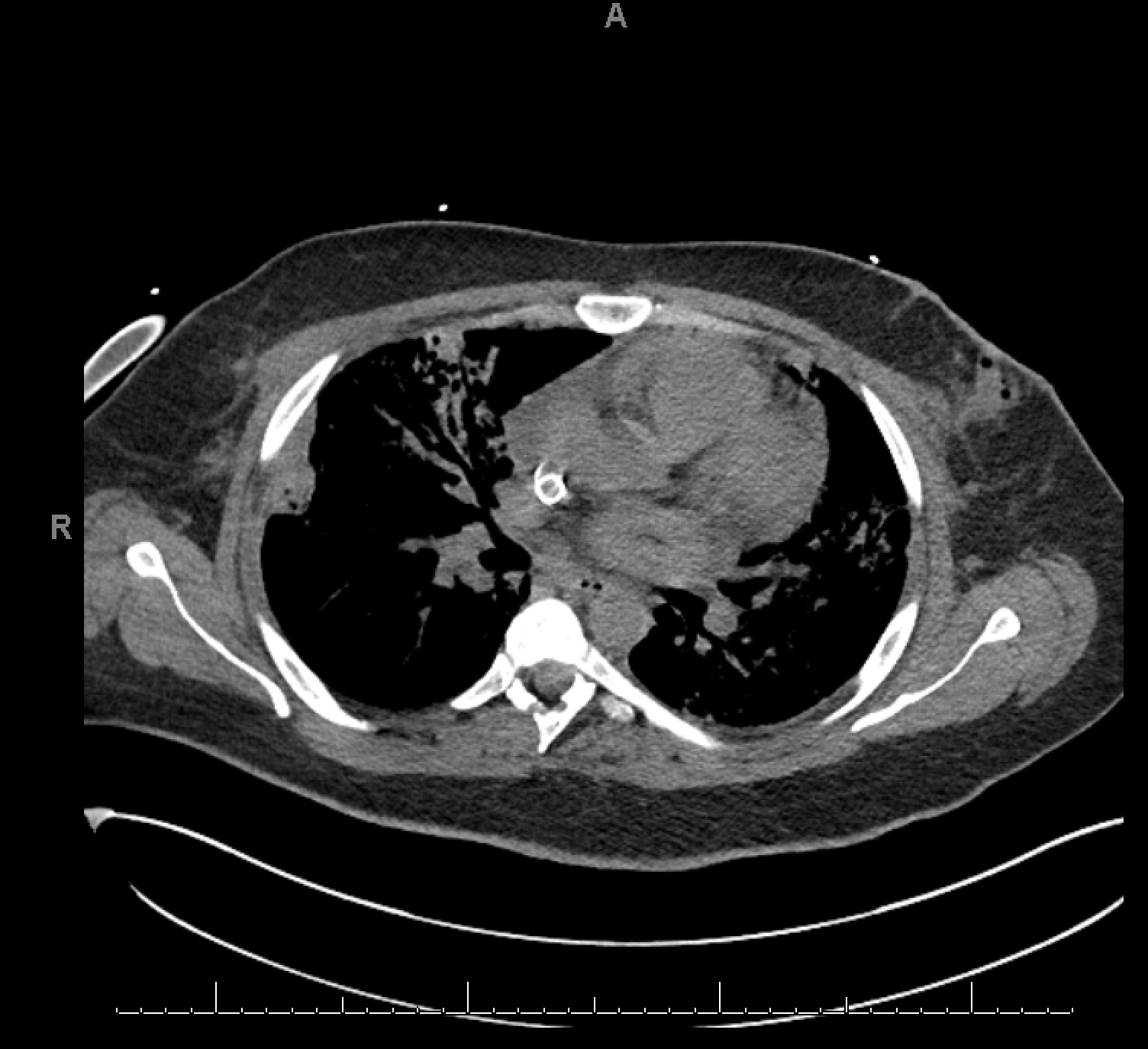
At this time, a computed tomography of the chest (Figure 1) was remarkable for complete opacification of the airways by blood. Laboratory data subsequently revealed elevated proteinase-3 antibody of > 8 (reference range <1) and elevated cytoplasmic ANCA (c-ANCA) titer of 1:320 confirming the diagnosis of granulomatosis with polyangiitis (GPA). The patient was treated with high dose methylprednisone, cyclophosphamide, and plasmapharesis with gradual improvement. He was extubated and weaned off ECMO on hospital days 8 and 12, respectively, with stable respiratory status and repeat imaging showing nearly complete resolution of prior opacification (Figure 2).
Discussion: GPA is a systemic necrotizing vasculitis affecting small to medium-sized vessels with involvement of the respiratory tract and kidneys. It is typically associated with anti-neutrophil cytoplasmic antibodies (c-ANCA), specifically to proteinase-3. GPA and other vasculitides can result in DAH due to inflammation of alveolar and capillary walls causing hemorrhage. DAH is a well-recognized clinical entity defined by hemoptysis, anemia, diffuse radiographic pulmonary infiltrates, and hypoxic respiratory failure. It is a rare and serious manifestation of GPA, occurring in approximately 5-10% of patients with a significant mortality risk of 60%, six times greater than vasculitis without pulmonary hemorrhage. In particularly severe cases, ECMO may be needed for adequate blood oxygenation when maximal mechanical ventilation is ineffective. Favorable outcomes have been reported for ECMO in GPA-associated DAH; it serves as a temporizing and life-sustaining intervention while immunosuppressive therapy takes effect.
Conclusions: GPA may present with severe DAH and potentially fatal hypoxic respiratory failure. One must maintain a high clinical suspicion for GPA in patients who present with hemoptysis, in the setting of other signs and symptoms of vasculitis. Given the rapid progression of DAH, it may be necessary to initiate aggressive empiric therapy while awaiting definitive diagnostic testing results.