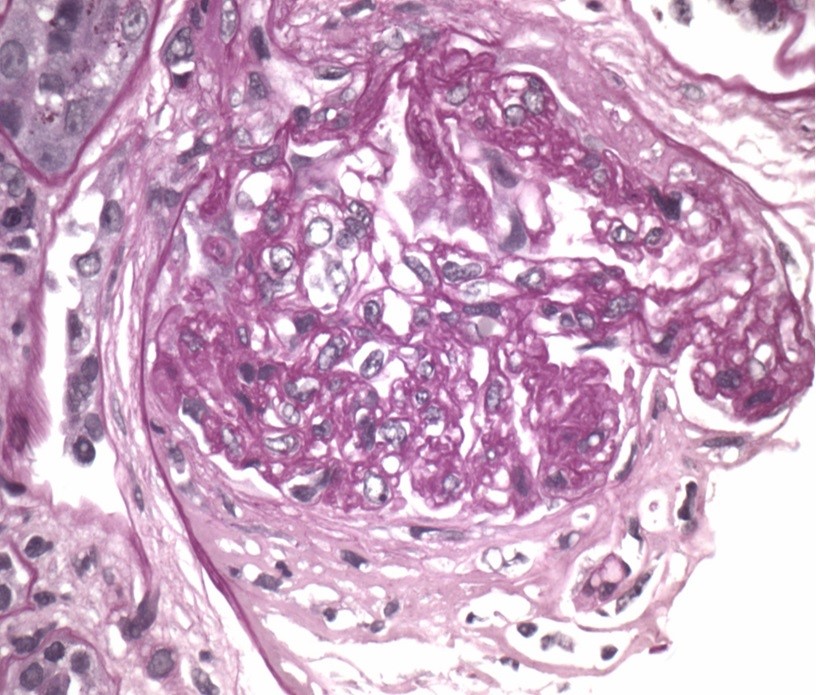
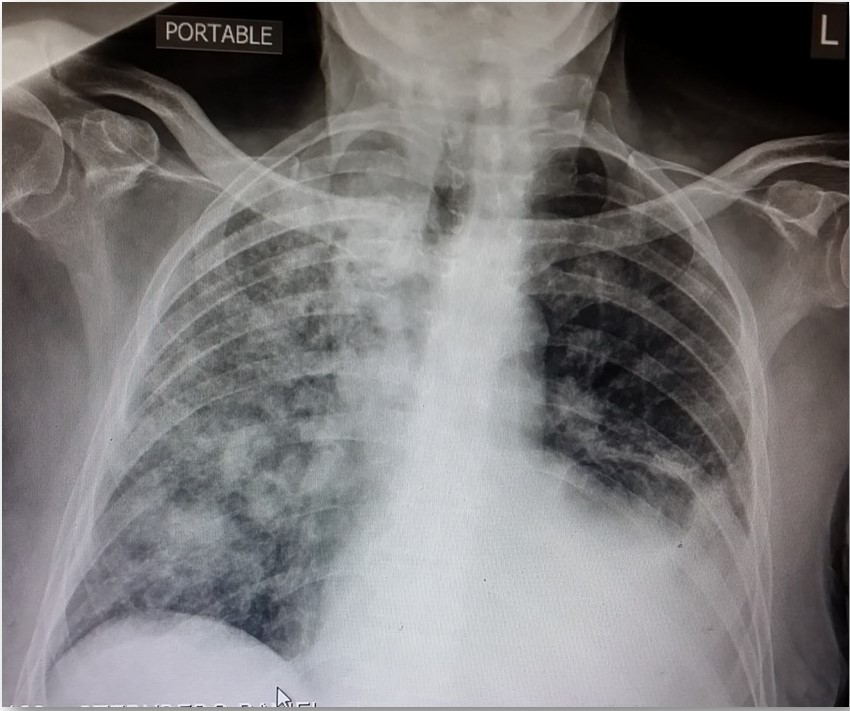
Case Presentation: 80-year-old man with a history of hypertension, atrial fibrillation, chronic kidney disease, multiple strokes with mild residual expressive aphasia and right hemiparesis presented with one week of dyspnea, fatigue and two days of worsened neurologic symptoms. His medications included nifedipine, metoprolol, coumadin and hydralazine since 2012. On exam, right arm pronation and decreased hand grasp were noted. CT-head was unrevealing. Testing showed hemoglobin 7.3 g/dL (baseline 14 g/dL), INR 4.0, creatinine 9.3 mg/dL, microscopic hematuria, non-nephrotic proteinuria and coarse granular casts. In the ED he developed acute respiratory distress with Spo2/FiO2 of 48. The chest imaging evidenced bilateral confluent ground-glass opacities. The patient underwent blood transfusion due to further drop in hemoglobin and received broad-spectrum antibiotics. Neurological deficit improved post-transfusion. A bronchoscopy revealed diffuse alveolar hemorrhage (DAH) with 80% neutrophils, required intubation post-procedure as respiratory distress worsened. Further workup revealed CRP of 122 mg/L and ESR of 65, initially normal C3 and C4 that subsequently decreased, dANA>1:2560-homogenous, positive anti-MPO, indeterminate RNP and Scl70 antibodies, negative rheumatoid factor, anti-GBM, anti-PR3 and cultures. Renal function deteriorated requiring permanent hemodialysis. Renal biopsy demonstrated focal extracapillary proliferative glomerulonephritis. The patient was treated with pulse steroids, plasmapheresis and Rituximab and was successfully extubated three weeks later. After a prolonged hospital course and rehabilitation he returned to the community.
Discussion: The presentation of this case is interesting since neurological deficits were manifested initially and while in the ED continued to unfold with acute respiratory distress and hypoxemia. Dyspnea and cough are nonspecific initial symptoms of DAH and like in this case, hemoptysis is absent in one-third of patients because the total alveolar volume is large and can absorb significant amounts of blood without extending more proximally into the airways.Drug-induced vasculitis (DIV) is predominantly an ANCA-positive small vessel vasculitis and unlike idiopathic vasculitis commonly produces various autoantibodies which may resolve spontaneously after discontinuation of the offending agent. One-third of patients with anti-MPO positive vasculitis have been exposed to hydralazine for months. Hydralazine-induced vasculitis has been described before but rarely causing pulmonary-renal syndrome.
The outcome of this octogenarian patient is remarkable as he survived despite several predictors of poor prognosis in vasculitis: age ≥80, initial creatinine >3.2 and respiratory failure with Spo2/FiO2<450, CRP >25, BAL neutrophils >30%. It has been reported that elderly patients have a better outcome if treated, particularly with Rituximab, but immunosuppressive therapy has not associated with renal survival like in this case.
Conclusions: DAH diagnosis requires a high level of suspicion since absence of hemoptysis is common.
Hydralazine is a known cause of DIV and can develop months after exposure.
Treatment with immunosuppressive therapy can provide good outcomes in the elderly, except for renal survival.