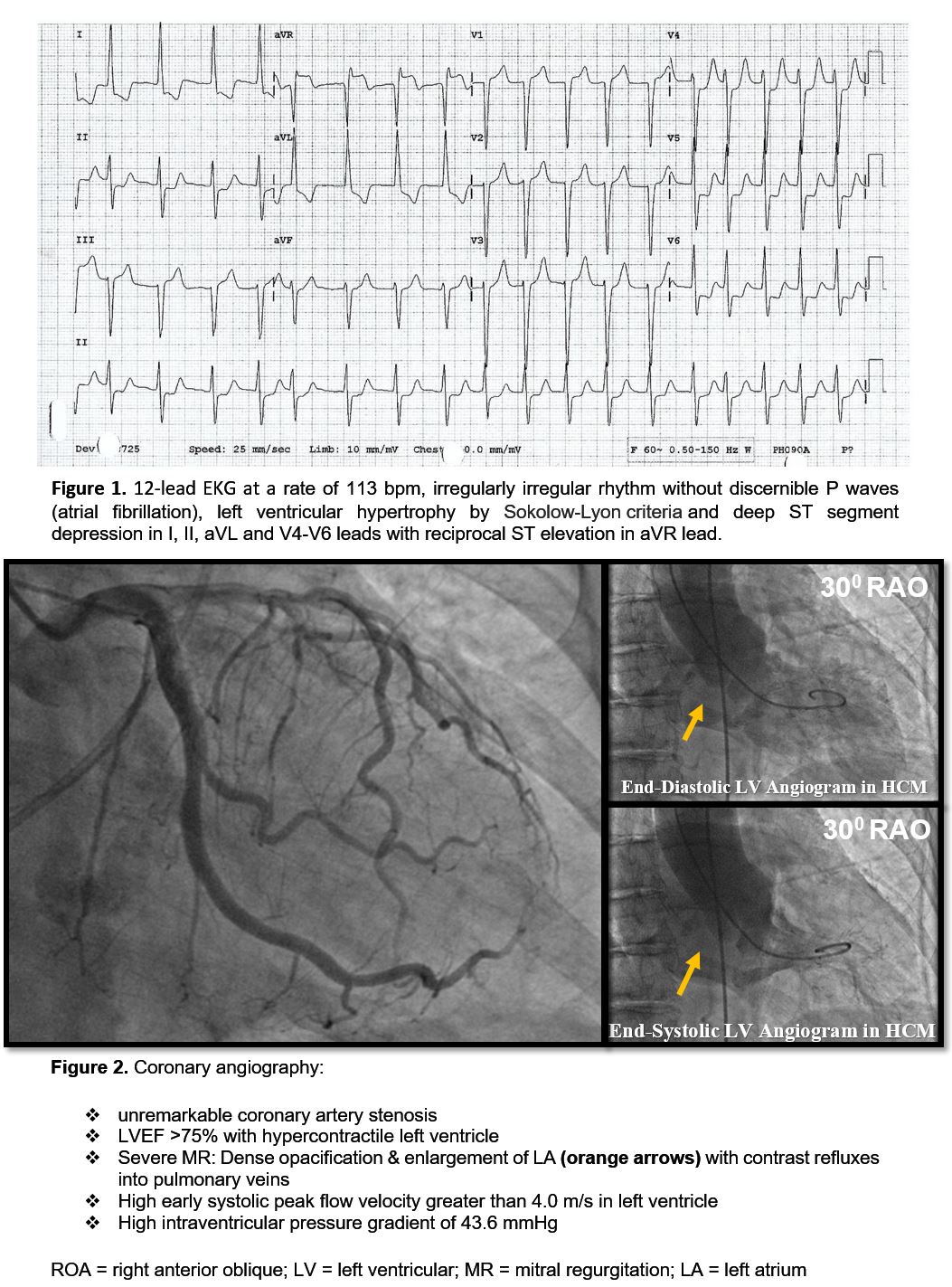
Case Presentation: ST-elevation in lead aVR, with ST-depression in precordial leads, has been reported to arise from left main coronary disease, often required emergent cardiac catheterization. We present a case of unstable SVT in a patient with hypertrophic cardiomyopathy (HCM) mimicking acute coronary syndrome (ACS) and cardiogenic shock. An 89-year-old female with paroxysmal atrial fibrillation and HCM presented with acute chest pain, palpitations, and dyspnea. Initial blood pressure was 138/77mmHg but shortly after arrival, she became hypotensive (55/37mmHg). Physical examination: weak peripheral pulses and grade III systolic murmur at left sternal edge. Electrocardiography (ECG) was as shown in Figure 1. Initial troponin was negative. Under the impression of ACS, she was given aspirin 325 mg and started on heparin and inotropic drips. An emergent electric cardioversion was performed to stabilize her hemodynamic status. Subsequently, a cardiac catheterization was performed which showed unremarkable coronary artery stenosis (Figure 2). Echocardiography showed high left ventricular outflow tract gradient of 71 mmHg. She was treated with optimal medical therapy (amiodarone, apixaban, Beta-blocker, and statin). She remained in sinus rhythm and chest pain-free prior to discharge with outpatient follow-up.
Discussion: HCM is an autosomal-dominant disease characterized by asymmetric areas of LVH. HCM, in the long run, will result in structural abnormalities of intramural coronary arterioles and may blunt myocardial blood flow (MBF) under stressful event. Literature has suggested that ST-elevation in lead aVR, with widespread ST-depression, could be a sign of incomplete left main coronary artery occlusion, proximal left anterior descending artery occlusion, severe multi-vessel disease or diffuse subendocardial ischemia. As in our patient, in the setting of atrial fibrillation, the cardiac output was reduced by 20-30%. In addition, acute dynamic left ventricular outflow tract obstruction with severe MR further suppressed the stroke output and led to a profound state of hypotension. Hence, the findings in the ECG were a result of diffuse subendocardial ischemia secondary to supply-demand mismatch.
Conclusions: This case highlights the importance of understanding the nature of HCM and remembering that such dynamic pattern of ECG changes is not always truly an ACS event.