Case Presentation:
A 34 year old man presented with five days of severe right eye pain. Hours after popping a pimple on the supraorbital ridge of his right eye, he developed fevers, chills, headache, blurry vision, and diplopia.
Vitals on admission were T–96.7OC, BP–125/86, HR–69, RR–18, 98% on RA. Exam was notable on the right side for proptosis, pain with extraocular movements, periorbital erythema, swelling, restricted upward gaze, and conjunctival injection. Fundoscopic exam was normal with intact visual fields.
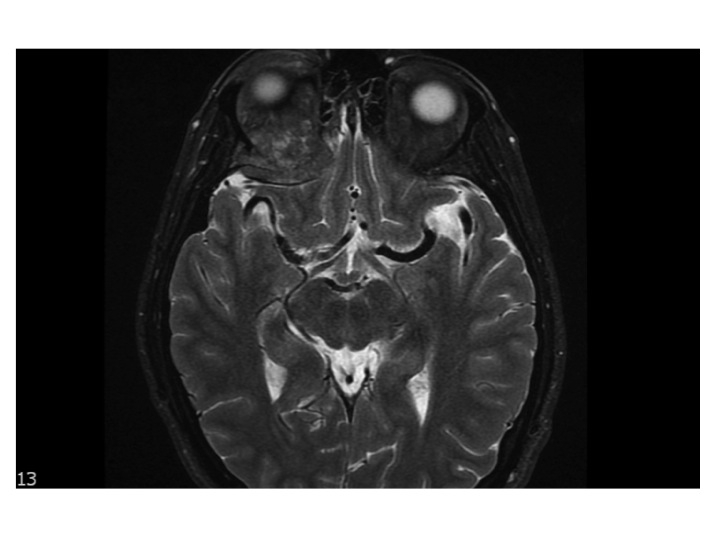
Labs were notable for a hemoglobin of 11 g/dL, MCV of 73, and iron saturation of 5%. Head CT to rule out orbital cellulitis revealed a calcified soft tissue mass in the deep posterior superior right orbit causing deviation of the superior rectus muscle inferiorly. Brain MRI re-demonstrated a 3 x 3.9 x 2.2 cm retro-orbital mass (IMAGE). Neurosurgery performed a right orbitotomy with tumor debulking and biopsy showing metastatic glandular carcinoma (IMAGE). Staging CT revealed multiple bilateral pulmonary nodules, numerous hypoattenuating liver lesions, and an area of rectal wall thickening with an enlarged left perirectal lymph node. Colonoscopy demonstrated a hemi-circumferential friable rectal mass located three cm from the anal verge (IMAGE). On further questioning, the patient reported intermittent rectal bleeding and rectal prolapse over the last year attributed to hemorrhoidal bleeding exacerbated by narcotic-induced constipation. There was no family history of malignancy.
Rectal mass biopsy showed moderately differentiated rectal adenocarcinoma with normal genetic markers. The patient underwent palliative radiation to the right eye and systemic chemotherapy with FOLFIRI & Bevacizumab but passed away eleven months after his initial presentation.
Discussion:
Although colorectal cancer is the third most common malignancy in men and women, metastases to the orbit are exceedingly rare with only eight cases described in the literature. Melanoma, breast cancer, and prostate cancer are the most common primary malignancies associated with orbital metastases. Of the eight reported cases, this case is unique in that the initial diagnosis was made after the patient presented with an ophthalmologic complaint.
Rectal cancer metastasizes via two known mechanisms, the portal venous route and the seeding of Batson’s venous plexus. One theory as to why orbital metastases are so rare may be the long distance through multiple vascular beds that tumor emboli must traverse to reach the eye. Orbital metastases from colorectal cancer have a poor prognosis as all reported patients died within one year of orbital involvement.
Metastatic rectal carcinoma most commonly occurs in older individuals or in younger patients with familial genetic abnormalities. The patient’s young age may be a reason why further workup for rectal bleeding was not initially pursued. Hospitalists commonly encounter rectal bleeding, and it is imperative that providers are able to differentiate life-threatening and malignant etiologies from benign conditions.
Conclusions:
This case illustrates the importance of obtaining a detailed history and physical while highlighting the perils of anchoring bias (i.e. attributing rectal bleeding to hemorrhoids in a young patient) that led to a delayed diagnosis of rectal cancer. In addition, this case is particularly noteworthy given the patient’s young age, negative family history, normal genetic markers, and unusual clinical symptoms that led to the diagnosis of metastatic cancer.