Background: The general medicine service at the Hospital of the University of Pennsylvania has recently undergone a significant restructuring with the addition of new teams and redesign of rounding workflow. Bedside interdisciplinary rounds now include the patient’s nurse, a pharmacist, clinical resource coordinator (CRC) and social worker, in addition to the medical team. We evaluated the effectiveness of the new rounding system in terms of nurse-physician communication and expediting early discharges, given institutional goals of improved patient flow.
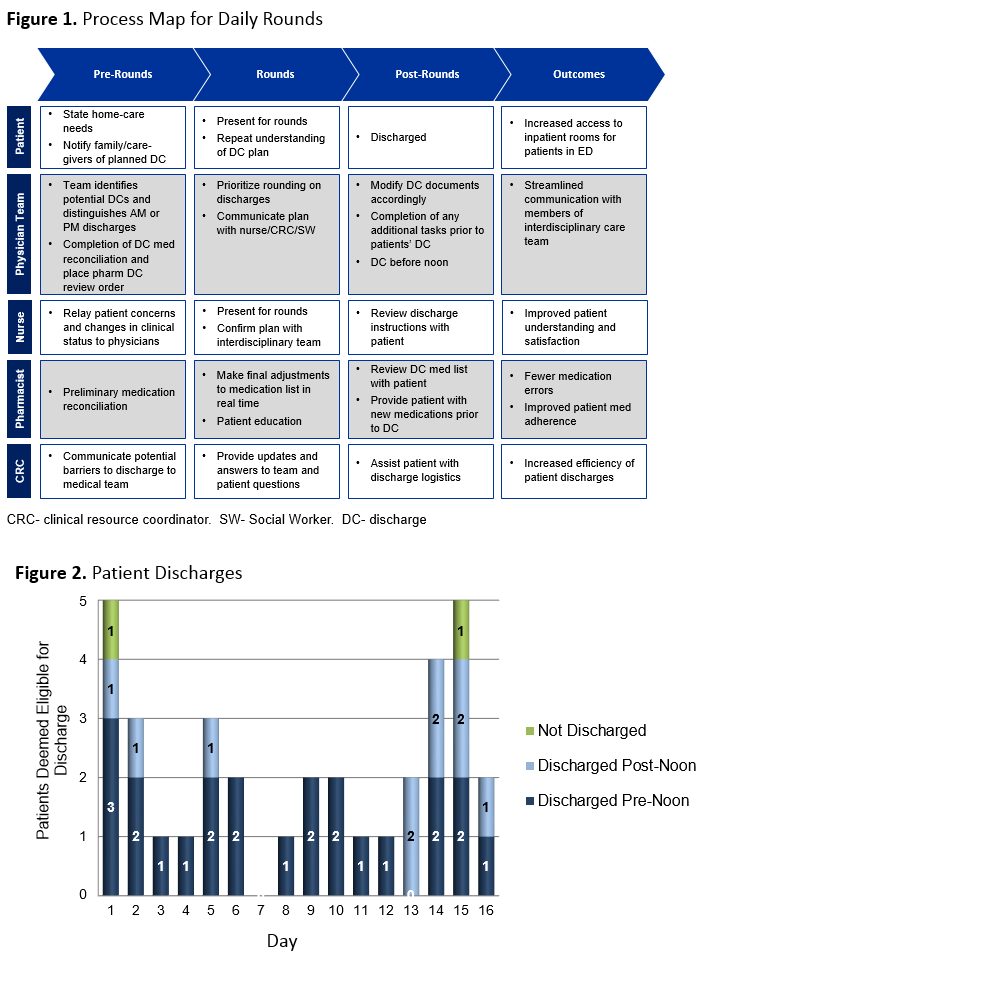
Purpose: Over a three week period (Nov. 11th– 27th, 2014), one of six general medical teams piloted a standardized protocol for daily rounds (Figure 1). Prior to the start of rounds, patients who were deemed eligible for discharge were prioritized for early rounds. Prior to seeing each patient, a secure text message was sent to each nurse asking that they join the team for rounds. The presence of the bedside nurse, clinical resource coordinator, social worker, and pharmacist was documented for every patient encounter. We then documented whether the identified patients were successfully discharged as well as if their discharge order was placed before noon.
Description: In 16 days, a total of 128 patient encounters occurred on rounds. Overall, a pharmacist was present in 68 (53.1%) cases, a CRC or social worker was present in 29 (56.9%) cases, and the patient’s nurse was present for rounds in 72 (56.3%) cases. In 33 cases (25.8%), the nurse was already at the patient’s bedside and did not require a text message. The patient’s nurse was text messaged for rounds on 93 patients, joining the team for rounds in 69 (74.2%) of cases, responding via text in 10 (10.8%) cases, and did not respond in 14 (15.0%) cases. During this interval, 36 patients were identified as discharge candidates, all but 2 were discharged that day, and 23 (63.9%) had discharge orders placed before noon (Figure 2).
Conclusions: Our newly implemented interdisciplinary rounding model shows promise for a high degree of physician-nurse communication and appears to effectively facilitate early patient discharge. Further study is planned.