Background: Health information technology (HIT) is promoted to improve the medication reconciliation process. However, the Multi-Center Medication Reconciliation Quality Improvement Study (MARQUIS) found an increase in potentially harmful medication discrepancies after HIT implementation. We explore how HIT design, implementation, and systems issues influence its successful use.
Methods: Five U.S. health systems with four different electronic health records (EHRs) participated in a two-year mentored medication reconciliation quality improvement study from September 2011 – June 2014. A toolkit of 11 medication reconciliation best practices included HIT implementation and optimization. Four of five sites made major HIT changes including new EHR deployment or improvements to medication reconciliation modules within existing EHRs. Staff views of HIT in the medication reconciliation process and systems issues impacting HIT use were elicited from front line staff interviews and focus groups. Content analysis of transcribed notes identified HIT challenges relating to design, implementation, and/or use and systems issues.
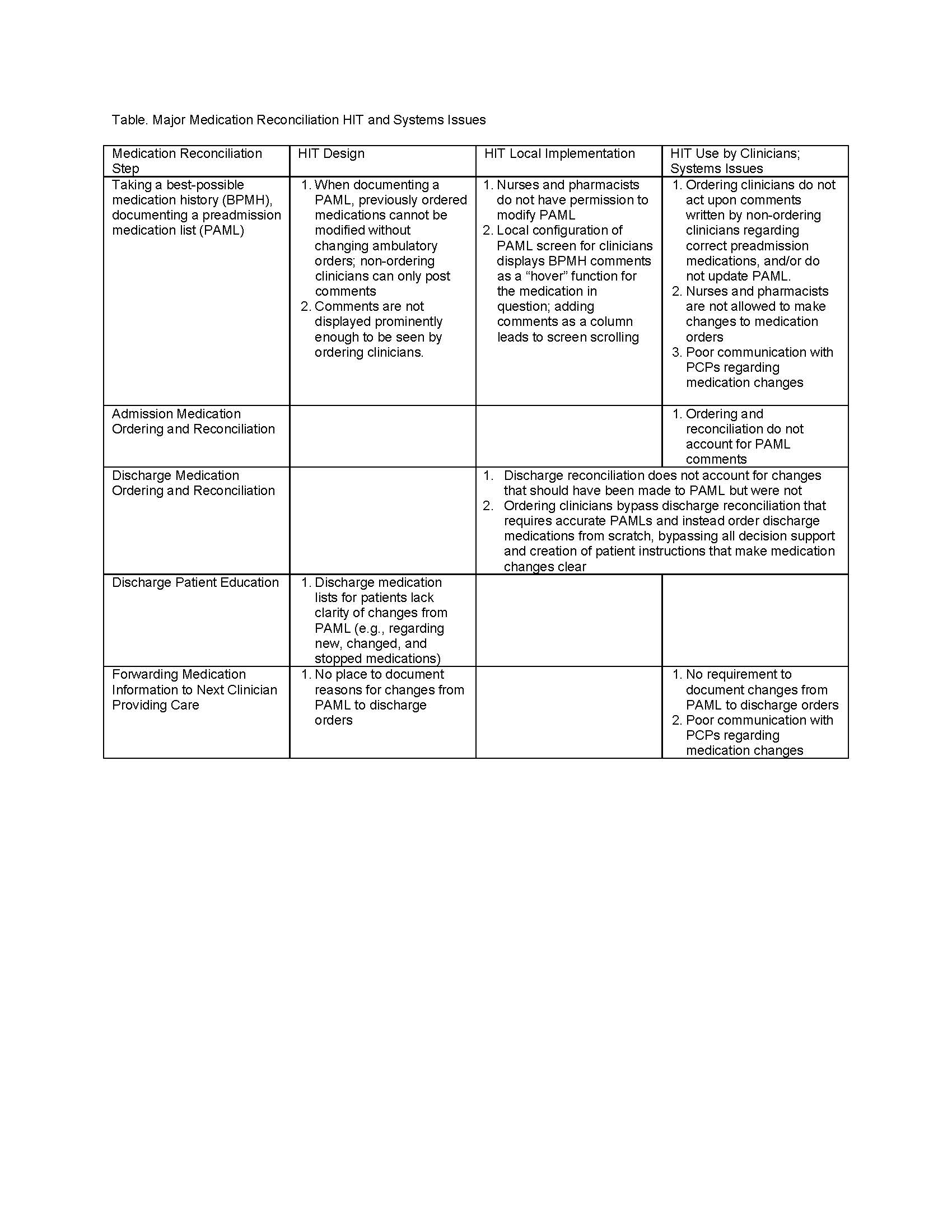
Results: Major HIT challenges were of several types, often interacting with each other (Table). For example, in some systems, due to design issues, preadmission medication lists (PAMLs) could not be modified without changing ambulatory orders from which the medications were derived; this often meant that nurses and pharmacists lacked EHR permission to make direct changes to PAMLs and instead left notes/comments. Physicians often did not see these comments, make corresponding changes to the PAML, or take action on them during admission reconciliation or medication ordering. In turn, this meant that discharge medication reconciliation did not account for changes that should have been made to the PAML but were not. Discharge patient instructions therefore lacked the ability to accurately document the changes in discharge medication regimens compared with the PAML, i.e., which medications were new, changed and discontinued. Systems issues included lack of coordination with referring physicians and lack of documentation of reasons for medication changes, both leading to inappropriate discharge orders.
Conclusions: Significant challenges exist with the design, implementation and use of HIT during medication reconciliation processes that together with systems issues, impact patient safety. Vendors, organizations, and HIT personnel should prioritize initial HIT design, local implementation and use and invest resources in optimization.