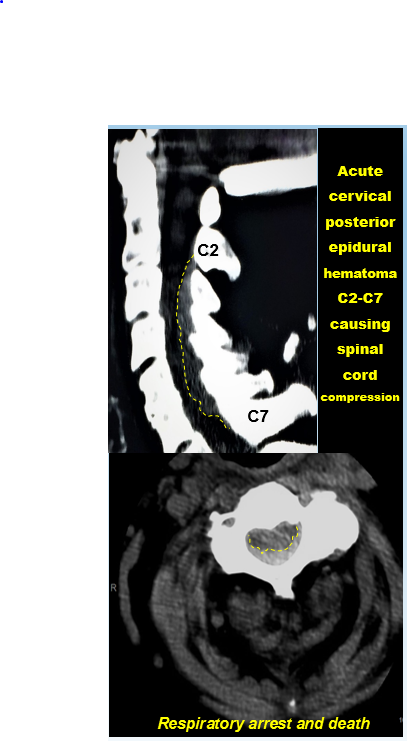
Case Presentation: A 90-year-old Caucasian female with non-valvular atrial fibrillation, on therapeutic anticoagulation with warfarin was admitted with community acquired pneumonia. She was treated with Levofloxacin. She underwent cardioversion for symptomatic atrial fibrillation with rapid ventricular rate and was later switched to Rivaroxaban 20 mg. Hepatic and renal function were within normal limits (creatinine clearance was 120 to 140 ml/min). After the second dose of Rivaroxaban, the patient developed acute onset of quadriplegia. Repeat INR was elevated to 6 and PT was 64.2 seconds. Computed Tomography scan of the neck revealed posterior cervical epidural hematoma from C2 to C7 with cord compression. Unfortunately the patient died shortly after.
Discussion: Rivaroxaban and warfarin are known to have a synergistic anticoagulant effect, usually seen shortly after switching. Antibiotics also increase the effects of warfarin by the inhibition of metabolizing isoenzymes. It is hypothesized that these two effects led to the fatal cervical spinal hematoma.
Clinicians are increasingly using rivaroxaban for the approved indication of thromboembolism prophylaxis due to its stable and predictable pharmacodynamics and pharmacokinetics that usually needs no laboratory monitoring. It interacts less with food or other drugs; causes less intracranial or fatal bleeding; and is overall non-inferior to Warfarin. There is paucity of data on how to safely switch from oral vitamin K antagonist (VKA) to Rivaroxaban. Expert opinion is to switch 24 hours after INR < 3. Single observational matched-cohort study of switching VKA to Rivaroxaban supports above mentioned practice. In another study of in silico effects, a post-switch synergistic anticoagulant effect has also been observed and a nomogram has been developed for switching to Rivaroxaban, based on INR for Caucasian and Japanese patients. INR is affected variably by Rivaroxaban and cannot be used as a marker for its anticoagulant effect.
Conclusions: Switching VKAs to newer direct oral anticoagulants (DOACs) is now becoming a common situation faced by clinicians, since the latter are thought to have a reduced incidence of intracranial bleeding. The current case report teaches us that the synergistic effect and interactions with antibiotics should be kept in mind during transition from VKAs to DOACs. Further studies are required to standardize bridging, duration and population-specific dosing. Laboratory monitoring of anticoagulant effect of DOACs needs to be considered, although INR is unsuitable for this.