Case Presentation:
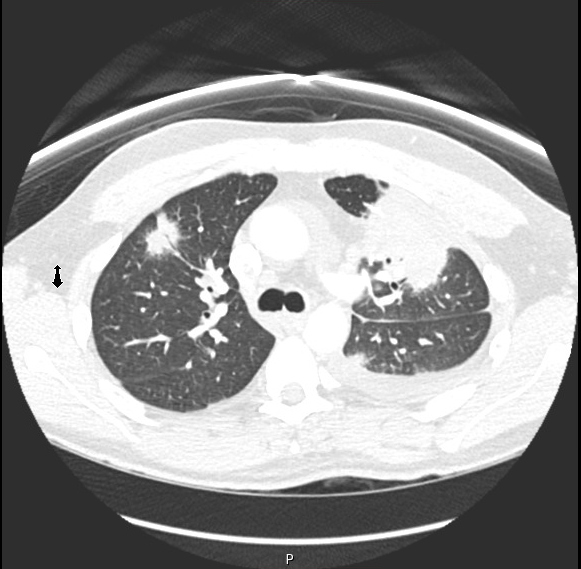
A 37-year-old man presented with fevers, chills, pleuritic chest pain, productive cough, and hemoptysis. He endorsed a six-month history of worsening cough, night sweats, and 25-pound weight loss despite a course of antibiotics followed by a course of steroids. His only pertinent social history was travel to multiple areas of East Asia and Singapore. Chest CT demonstrated left upper lobe pulmonary consolidation, right upper lung nodule, scattered airspace opacities, and a dominant cavitary lesionin the lingula. Laboratory investigation revealed elevated ESR and CRP with negative infectious and autoimmune workup. CT guided biopsy of the right upper lobe nodule and left sided thoracentesis were negative for malignancy and infectious agents. Pathology from the biopsy demonstrated non-caseating granulomas. Patient subsequently underwent video assisted thoracoscopic right lower lobe wedge resection for confirmatory tissue diagnosis, with pathology again demonstrating caseating and non-caseating granulomas and negative microbiologic studies. Patient was initiated on high dose steroids with plan for taper; however given lack of treatment response, infliximab was initiated with considerable clinical improvement and subsequent decrease in prednisone dose to 10 mg/day.
Discussion:
This case highlights the difficulty in arriving at a confident diagnosis of sarcoidosis when the disease presents with atypical pulmonary manifestations – cavitary lesions, mass lesions, and pleural effusions. It demonstrates that sarcoidosis remains a diagnosis of exclusion and requires a thorough work up to rule out infectious and autoimmune diseases.
Conclusions:
While steroid therapy usually results in prompt clinical improvement in patients with sarcoidosis, a lack of response to such therapy does not exclude the diagnosis, and other immunosuppressive strategies can be effective in this setting.