Background:
Most patient arrivals at hospitals are unsynchronized with their discharges. If beds are assigned on a first come, first served basis, the result is patients being dispersed among several nursing units. This geographical disconnect results in decreased physician efficiency and decreased provider as well as patient satisfaction. However, holding patients in the emergency department (ED) for beds to become available in an “appropriate” nursing unit may lead to the buildup of a “queue” of patients in the ED and adversely affect throughput. Queuing theory, from the discipline of decision analysis, is specifically suitable for evaluating and optimizing random processes such as these.
Purpose:
The goal of the study was to use queuing theory to establish geographically localized hospitalist units and to evaluate their impact on hospital throughput.
Description:
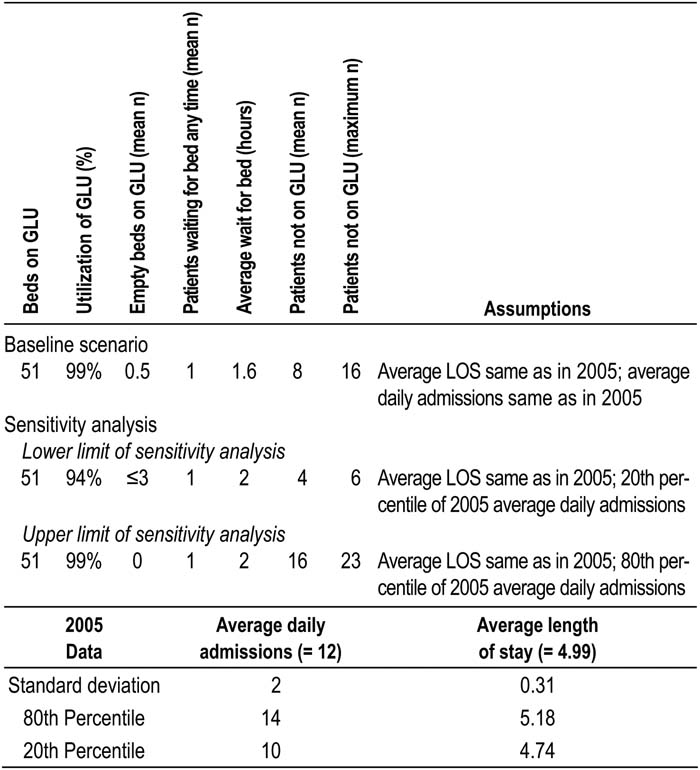
Hospital processes were divided into 2 main categories: nursing floors and the ED, where patients are held until a medical bed is assigned. For some of the internal medicine (IM) services, length of stay (LOS) data were reviewed and the numbers of IM admissions per hour were tabulated. Physicians were interviewed to determine the average number of IM patients in the ED awaiting bed assignments. Simulations using queuing theory were run with the intent of finding the optimal balance among average geographically localized unit (GLU) size, average wait time for bed assignment, and average bed capacity utilization on geographic units. Simulations showed that given the operational data, a GLU with 51 beds may be established for these medical services with 99% bed utilization. The average number of patients waiting in the ED would be 1, with a wait time of 1.6 hours. The number of patients not on a GLU would be 8/59, or 14%. Upper and lower limits of bed utilization and ED wait time were calculated using extreme values of operational data. Geographically localized IM units were established with bed capacity utilization over 6 months concordant with simulation results. No ED staff discontent with bed assignment wait time was noted.
Conclusions:
Capacity requirements for a geographically localized clinical unit and its impact on hospital operations may be evaluated using queuing theory.
Author Disclosure:
A. Usmani, None; A. Rajamanickam, None; S. Suri, None.