Case Presentation:
A 52 yo AA female presented with SOB, cough productive of green sputum and a 12lb weight loss over 3 months. PMH: AIDS (CD4 180), hx pulm TB (treated, yrs ago), DM2, ex-IVDU (heroin) on MMTP and a 40 pack-year tobacco hx.
PE wnl except: pulse ox 91% on 4L nc and rhonchi in the b/l lung fields. No lymphadenopathy appreciated.
Labs: Na 130 mmol/L, WBC 8.9 K/uL 89% neutrophils, Hgb 9.0 g/dL, MCV 75 fL and LDH 3604 U/L. Bld cxs neg x 2. AFB sputum cxs neg x 3.
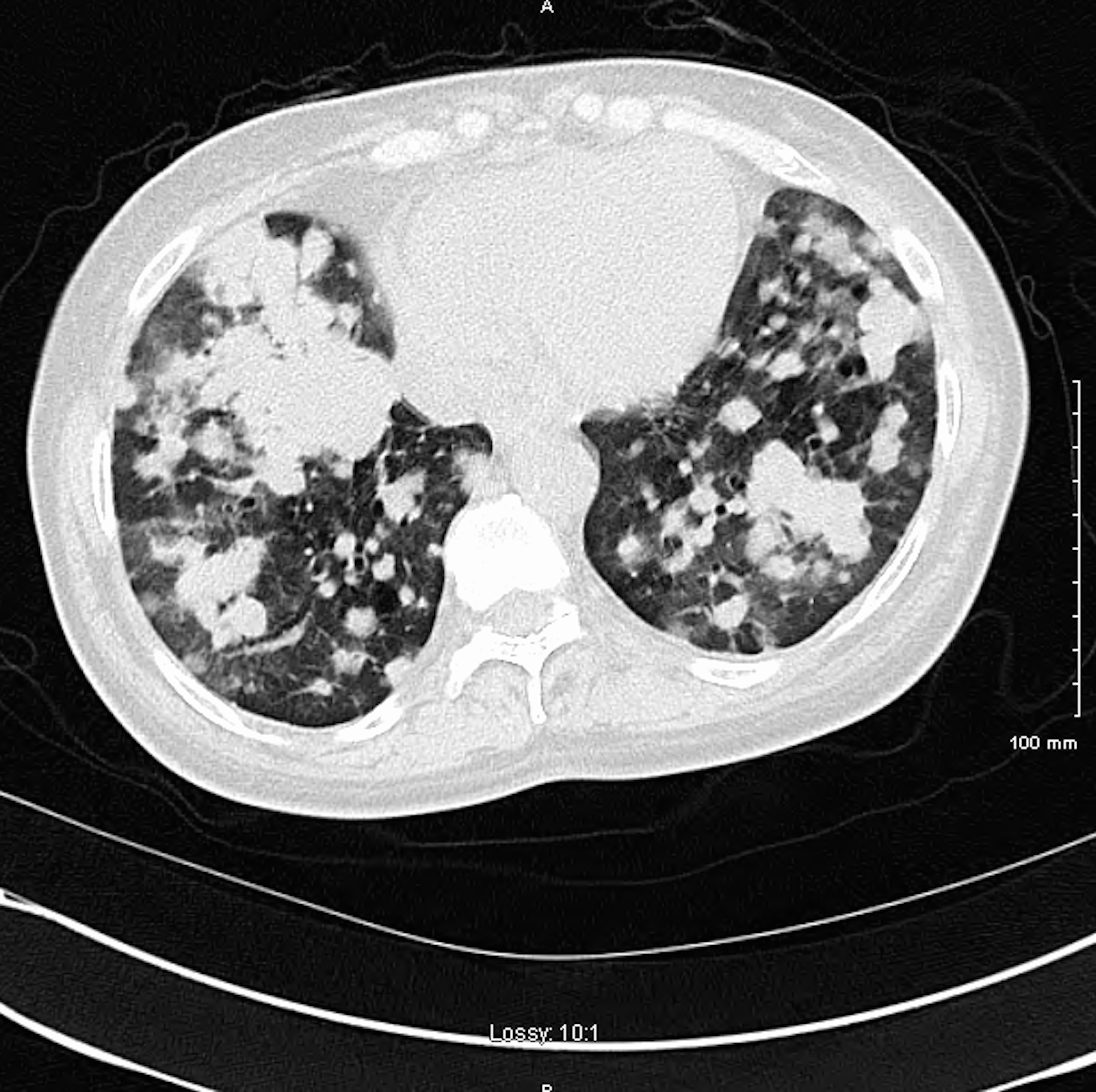
CT chest: Innumerable round, solid nodules in bilateral lung fields.
The patient was empirically treated for HCAP and pneumocystis jirovecii. The pt’s SOB improved modestly, still requiring 2L nc. A bronchoscopy with blind transbronchial biopsies of the pulmonary nodules was performed. Tissue analysis revealed: small focus of atypical cellular infiltrates/immunophenotypic features c/w diffuse large B-cell lymphoma (DLBCL). Immunohistochemical stains showed the cells co-expressed CD20, CD10, Bcl-2 and Bcl-6 markers with markedly elevated proliferative activity as demonstrated by Ki-67 stain. Fungal stains for pneumocystis were negative. A bone marrow biopsy revealed no lympho-proliferative process. The pt’s RI Prognostic Index was calculated to be ‘poor’ with a predicted 4 year progression-free survival of 53% and overall survival of 55%. The pt declined a CT abdomen/pelvis, MRI brain, LP and chemo and left AMA.
The pt shortly returned to the hospital in severe respiratory distress. A repeat CT chest, 17 days from the original CT, revealed rapid progression of the pulmonary nodules as well as nodules in the kidneys, liver and spleen. She was transferred to the ICU, but declined intubation. The pt accepted comfort care measures only and was transferred to the hospice unit. She passed 2 days later. Clinical course from presentation to death=22 days.
Discussion:
DLBCL accounts for 25% of all non-Hodgkin’s lymphoma in the United States. Although extranodal involvement can be found in up to 26% of cases on presentation, primary pulmonary involvement accounts for only 8% of these extranodal cases and only 2% of total cases. Additionally, pulmonary involvement is usually manifested as central (single or multiple) nodules, size greater than 1cm. It is rare to see diffuse innumerable bilateral pulmonary nodules as the initial presentation of diffuse large B-cell lymphoma as our case illustrates.
B-cell lymphoma/NHL may be a late manifestation of HIV, with rates rising with the length of time infected. Pts with HIV associated NHL present with advanced disease and/or extranodal disease commonly. Most common site is the GI tract with hepatic involvement in a quarter of the patients. Pulmonary involvement is not commonly seen.
Conclusions:
Lymphoma should be considered in the differential diagnosis of lung nodules, particularly in the immunocompromised patient.