Case Presentation:
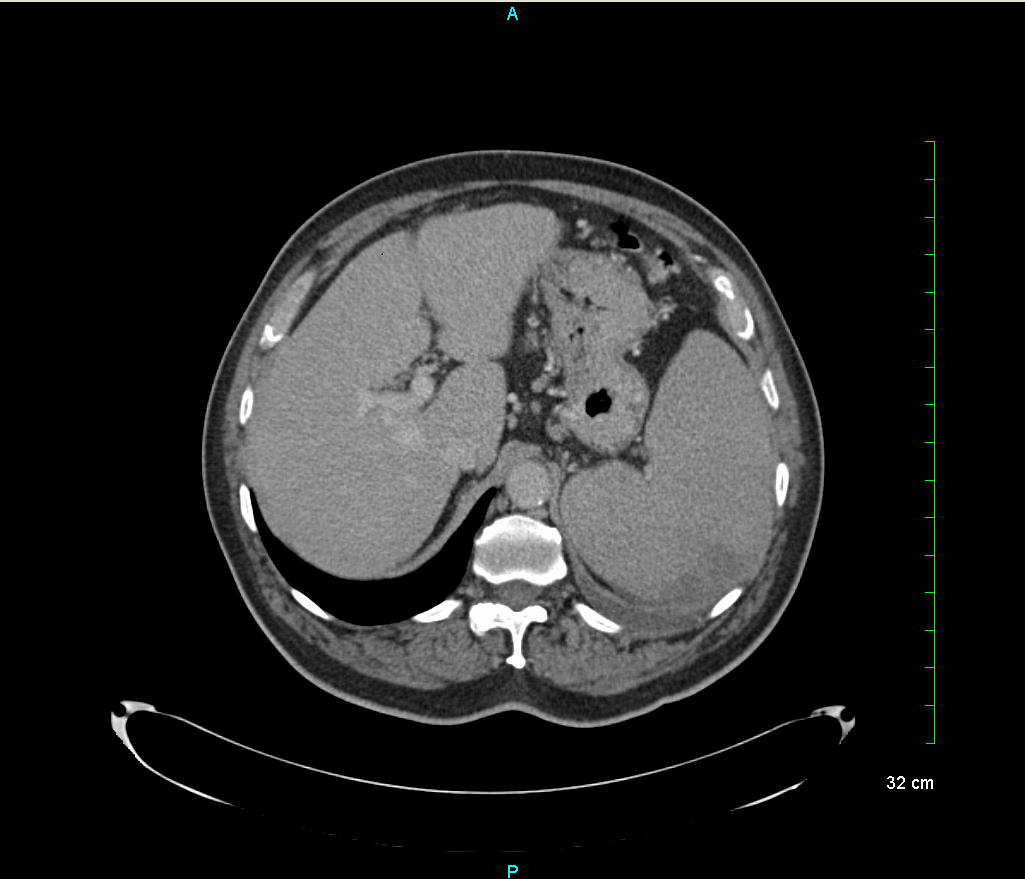
A 79 year old Hispanic male with a past medical history of prostate cancer in remission, hypertension and hyperlipidemia presented with fever and left upper quadrant pain. The left upper quadrant pain began two weeks prior to presentation during an aggressive exercising session, was sharp and without radiation. Associated was five days of fever, for which he took left over Bactrim but due to the progression of his symptoms, presented to the emergency room for evaluation. He denied weight loss, shortness of breath or hemoptysis. A CT scan was performed and demonstrated a 1.3cm hypodense thyroid nodule, 4mm calcified granuloma, splenomegaly to 15cm, a wedge shaped defect posteriorly in the spleen suggestive of infarction and multiple small mediastinal, porta hepatitis, left hilar and axillary nodes. The patients was tested for hepatitis, HIV, hypercoagulable diseases, opportunistic infections and had a transesophageal echocardiogram, which were all unremarkable. Blood work demonstrated anemia with a hemoglobin of 8.1 g/dL and an LDH of 859 U/L. An axillary lymph node biopsy was performed as a possible malignancy remained in the differential and results later confirmed mantle cell lymphoma, a new primary neoplasm. He was subsequently discharged home with supportive care and Rituxan was initiated as an outpatient.
Discussion:
Splenic infarctions occur when the splenic artery or its sub-branches become occluded with an embolus. Clinical presentation includes acute left upper quadrant pain, fever, leukocytosis, nausea and vomiting. The differential diagnosis for a splenic artery infarction is vast and simple cases are managed with local symptomatic control and anticoagulation when indicated. It is important to diagnose the primary cause as the complications of splenic infarctions include abscess, splenic rupture and pseudocysts. In this patient’s case, his diagnostic workup on admission did not reveal a diagnosis. A lymph node biopsy was performed to evaluate for malignancy as there were multiple possible primary neoplasm sites and none of the lymph nodes met pathological criteria for lymphoma. The patient is currently doing well s/p diagnosis and treatment of his malignancy.
Conclusions:
Splenic Infarcts are an uncommon phenomenon with a multitude of causes. It is vital to identify the cause of this phenomenon to prevent morbidity and mortality as it is usually the presentation of a larger disease entity.