Case Presentation:
A 66-year-old female with a history of rheumatoid arthritis on infliximab developed acute onset expressive aphasia and was diagnosed with a transient ischemic attack after a noncontrast CT head was negative. During this time, she developed a corneal abrasion which was complicated by dendritic keratitis followed by infections with staphylococcus epidermidis and yeast. With her active infection, ophthalmology held her infliximab until deceased donor corneal transplant several months later. Following her transplant, her neurologic symptoms and eye infection resolved and she was restarted on infliximab. Soon after resuming treatment, she developed intermittent episodes of lower extremity numbness followed by another episode of expressive aphasia prompting further neurologic evaluation.
On admission, her infliximab was held and MRI brain illustrated abnormal T2/FLAIR in bilateral frontal lobes and temporal lobe with leptomeningeal enhancement consistent with cerebritis. A lumbar puncture illustrated a lymphocyte predominant pleocytosis and an extensive infectious and neoplastic analysis of her cerebrospinal fluid (CSF) was unremarkable. Unfortunately, her clinical status continued to decline and she developed altered mental status, urinary incontinence, lower extremity paralysis and ultimately status epilepticus over the next several days. Serologic workup illustrated a positive rheumatoid factor and anti-CCP. Repeat lumbar puncture illustrated an elevated CSF rheumatoid factor. Brain biopsy of the dura and cerebral cortex illustrated abundant T-lymphocytes and macrophages consistent with hypertrophic pachymeningitis. Given her negative infectious workup and poor response to previous medical therapies, she was started on high dose steroids with rapid improvement in her symptoms.
Discussion:
Our patient’s negative infectious workup, elevated CSF rheumatoid factor and brain biopsy results are consistent with a diagnosis of rheumatoid meningitis. A recent retrospective analysis illustrated an increased incidence of aseptic meningitis in patients on tumor necrosis alpha (TNF-a) inhibitors compared to alternative disease modifying antirheumatic drugs. Our case is particularly unique in that our patient’s neurologic symptoms improved when infliximab, a TNF-a inhibitor, was held due to active infection and resumed following reinitiation of therapy.
Conclusions:
Rheumatoid meningitis is an exceedingly rare manifestation of rheumatoid arthritis. Though uncommon, there are a handful of case reports of rheumatoid meningitis developing in patients on TNF-a inhibitor therapy. With the current trend towards early and long term treatment with immunomodulating agents, over half a million patients have been treated with TNF-a inhibitors worldwide. Our case report highlights a unique clinical presentation and encourages physicians to carefully consider autoimmune etiologies for neurologic symptoms in patients on TNF-a inhibitor therapy.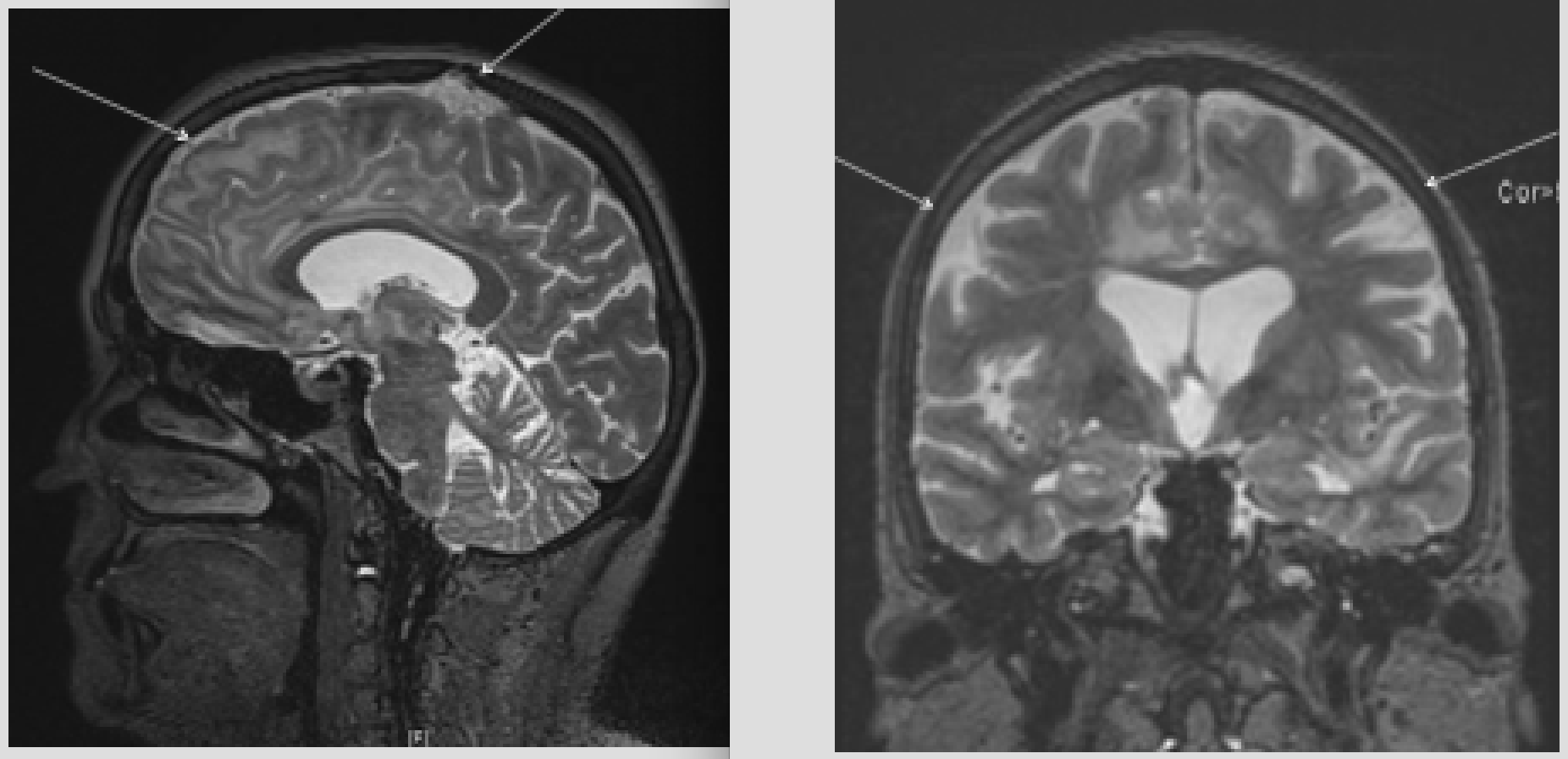
To cite this abstract:
The Shaky Side of Infliximab: A Case Report of Rheumatoid Meningitis Associated with Infliximab.
Abstract published at Hospital Medicine 2016, March 6-9, San Diego, Calif..
Abstract 786Journal of Hospital Medicine, Volume 11, Suppl 1.
https://shmabstracts.org/abstract/the-shaky-side-of-infliximab-a-case-report-of-rheumatoid-meningitis-associated-with-infliximab/.
April 23rd 2024.
