Background:
There is growing recognition that engaging patients/caregivers in self‐management will improve outcomes and lower costs. This is particularly important in the acute care and post‐discharge setting–new treatments have been initiated, conditions require close monitoring, and care plans are in flux. However, patients/caregivers often receive
conflicting information and inconsistent education
about their care plan. The fragmented dialog that transpires among care team members contributes to
a chaotic communication space.
Lack of a clear care plan that accurately reflects patients’ goals, priorities, and preferences can contribute to poor patient‐reported outcomes, suboptimal utilization of healthcare resources, and overall poor‐quality care. To promote meaningful engagement, healthcare systems must provide tools to patients/caregivers that facilitate patient‐specific education and seamless communication and collaborationbetween patients and their care team members across care settings. Our prior work outlines the core‐set of information tools provided via web‐enabled bedside devices to engage patients and caregivers in recovery–current patient‐facing portals are not optimized for the acute care and transitions settings, and rarely engage patients/caregivers in establishing goals, priorities, and preferences with regard to their care plan.
Purpose:
We report progress on a $2 million grant from the Gordon and Betty Moore Foundation to develop, implement, and evaluate a web‐based patient‐centered toolkit (PCTK), a component of the BWH PROSPECT (Promoting Respect and Ongoing Safety through Patient‐centeredness, Engagement, Communication, and Technology) initiative.
Description:
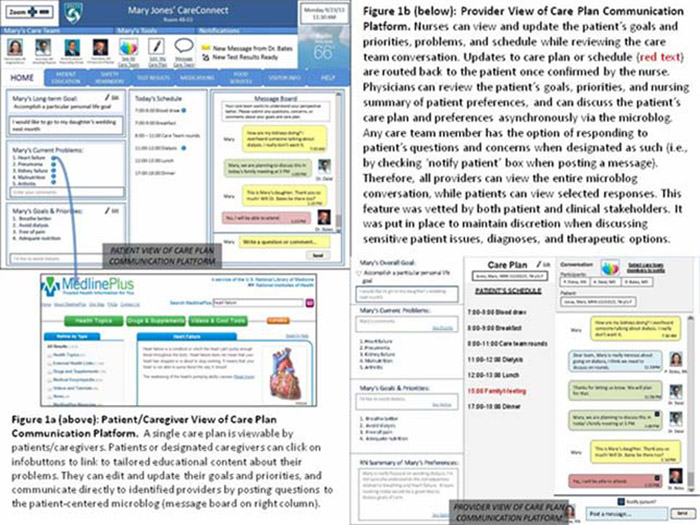
The PCTK provides patients/caregivers with tailored information presented at a consumer level of health literacy and the ability to seamlessly communicate with their care team members. We use structured coded data from the electronic health record and infobuttons® to support tailoring of education to the patient’s conditions, test results, and medications. Using an iterative, participatory design process involving key stakeholders, we have enhanced the PCTK to include a web‐based communication platform that allows patients/caregivers to view their care plan, establish and prioritize goals, and communicate directly to their care team members via a patient‐centered microblog. The PCTK is accessible via any web‐enabled device. To date we have engaged key stakeholders (nursing, physician, and clinical informatics leadership; patient and family advisory council members) to identify educational content, capture key care plan data elements, enhance usability, and facilitate workflow redesign. We are enrolling 4500 patients admitted to randomized intensive care, oncology, and medicine units. Baseline patient‐provider concordance with regard to patient’s main concern is 52%, suggesting much room for improvement.
Conclusions:
The web‐based PCTK has been well received by patient advocates, administrators, and nursing/physician leadership. All agree it has much potential to transform the acute care environment, which we attribute to our efforts at engaging key stakeholders. Our rigorous evaluation should provide valuable information with regard to impact on care plan concordance, adverse events, and healthcare resource utilization.