Case Presentation:
An 80 year old male with a medical history of Diabetes Mellitus Type 2, Hypertension, DVT + Pulmonary Embolism presented to the ED with difficulty walking, muscular weakness, increased frequency of falls associated with worsening dizziness over the past two weeks. Upon presentation to the ED, his physical exam revealed diminished tactile sensation over the right upper and lower extremities, slurred speech, right-sided hearing loss, and unsteady gait.
The patient’s family and social history were non-contributory. He had no-known drug allergies. Home medications included Rivaroxaban, Metformin, Glyburide, Atorvastatin, Tamsulosin, and Finasteride. Vital signs upon presentation were normal. Initial lab work including an SMA-7, CBC, PT/INR, and TSH were normal. HbA1c was 8.6.
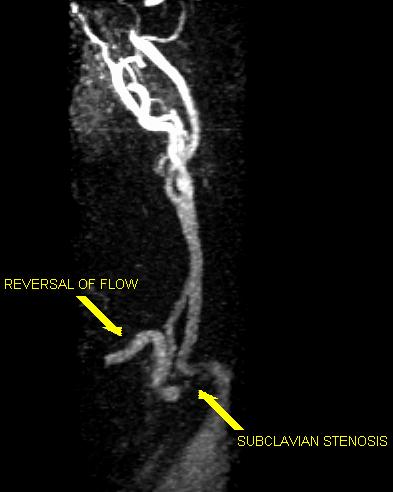
CT Head and MRI brain were negative for acute stroke and a transthoracic echocardiogram was normal. Carotid ultrasound revealed reversal of flow during systole in the right vertebral artery. MRA neck showed evidence of right-sided subclavian steal syndrome. After consultation with vascular surgery, the patient was discharged home with a plan for a staged endovascular subclavian stenting as an outpatient.
Discussion:
Most cases of subclavian steal syndrome are asymptomatic with most diagnoses occurring as incidental findings. Sometimes subclavian steal can present with symptoms due to ipsilateral upper extremity weakness. Symptoms from vertebrobasilar ischemia are even rarer and usually occur in patients who have a second intra-cerebral lesion. Our patient had symptoms of cerebral ischemia due to subclavian steal syndrome with no secondary intracerebral lesion.
Conclusions:
Subclavian steal syndrome should be considered in patients who are admitted for transient ischemic attacks or strokes of unclear etiology.