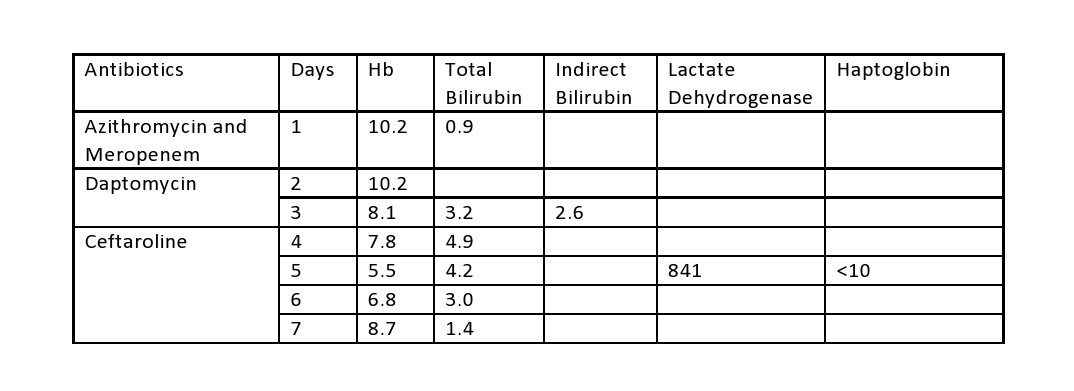
Case Presentation: A 35-year-old male with past-medical-history significant for cerebral palsy and ventriculoperitoneal shunt for ventriculomegaly was admitted with fever. Patient had completed a course of levofloxacin before admission. Patient was started on azithromycin and meropenem, for possible aspiration pneumonia, because of penicillin allergy. He continued to be febrile with elevated leukocytes despite antibiotics. Considering patient’s history of VP shunt, Infectious Disease (ID) was consulted and antibiotics were switched to daptomycin given possibility for VP shunt infection and Vancomycin allergy. Hemoglobin (Hb) was 10.2 and total bilirubin was 0.9 prior to starting daptomycin. After initiation of daptomycin, Hb declined to 8.1 and total bilirubin increased to 3.2 (indirect bilirubin was 2.6 and direct bilirubin 0.6). LDH was elevated at 841 and haptoglobin was <10. Patient had no prior history of hemolytic anemia. Direct Coombs test was performed which came back positive. Daptomycin was discontinued for possible daptomycin-induced Autoimmune Hemolytic Anemia (AIHA). Hematology was consulted and patient was started on oral steroids and ID changed antibiotic to ceftaroline. Patient’s hemoglobin and erythrocytes started improving afterward and total bilirubin trended down to 1.4.
Discussion: Drug-induced hemolytic anemia is very uncommon. It can be caused by various medications including antibiotics. The first incidence of hemolytic anemia was reported in 1954 with stibophen. It can be either immune or non-immune mediated. In immune type, drug-dependent autoantibody formation occurs which causes hemolysis. With non-immune type, hemolysis occurs with oxidant injury. In an asymptomatic patient, stopping the offending agent inciting hemolysis generally helps improve hemoglobin levels and no further intervention is required. In symptomatic patients, steroids or blood transfusions may be necessary in addition to the cessation of offending agents, depending upon the severity of the disease. Some case series showed that antibiotic-induced hemolytic anemia is commonly related to beta-lactam antibiotics like penicillin and cephalosporins. Daptomycin is a lipopeptide antibiotic and has been used for treating bacteremia, endocarditis, and skin/soft tissue infections. It works effectively against methicillin-resistant Staphylococcus aureus by disrupting bacterial cell membranes and affecting nuclear synthetic function. It has been used as a potent alternative for vancomycin. Overall, daptomycin has a good safety profile, albeit it can cause severe side-effects including eosinophilic pneumonia, myopathy, rhabdomyolysis, acute renal failure, and anaphylaxis. Thus far, one case study has reported for possible daptomycin-induced AIHA. Our case report presents another instance of daptomycin-induced hemolysis and its management.
Conclusions: Daptomycin is a very effective antibiotic for its approved indications. Considering the increasing use of daptomycin, we suggest that clinicians be cognizant of AIHA while using daptomycin and treat it appropriately should it occur.