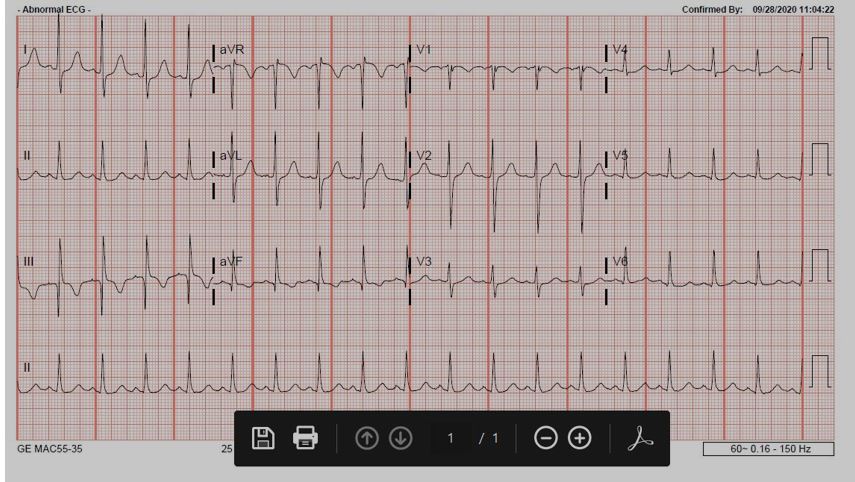
Case Presentation: A 53-year-old male with a past medical history of alcohol abuse presented to the emergency department after a presyncopal episode following new onset of hematemesis and black, tarry stools. He additionally had sharp, bilateral chest pain that was present at rest with no radiation or worsening with exertion. Upon presentation he was hypotensive, tachycardic, and tachypneic with labs significant for a hemoglobin of 3.8g/dl, serial troponins < 0.01ng/mL, and a d-dimer of 1.78mcg/mL. Electrocardiogram (ECG) showed sinus tachycardia with an S wave in lead I and aVL, Q wave and inverted T wave in lead III, and an incomplete right bundle branch block (figure 1). Specifically, the S1Q3T3 pattern in association with the elevated d-dimer and chest pain prompted urgent CTA of the chest which was notably with no pulmonary embolism (PE). He was admitted to the intensive care unit, and after receiving fluids and five units of pRBCs, a repeat ECG showed resolution of this S1Q3T3 phenomenon (figure 2). Echocardiogram the following day additionally showed evidence of right heart strain with an enlarged RV (3.8cm) in addition to a mildly dilated LV cavity (59mm) with an EF of 50-55%. Endoscopy showed grade 2 varices, portal hypertensive gastropathy, and multiple non-bleeding ulcers. Colonoscopy showed two angiodysplasias that were subsequently coagulated and clipped. On discharge, his hemoglobin was stable, and he had complete resolution of his chest pain and presyncopal symptoms.
Discussion: The McGinn-White sign or, more commonly known as S1Q3T3 pattern, is a nonspecific finding associated with right heart strain1. A common misconception is the sole association of this sign with a pulmonary embolism, which is just one possible etiology of right heart strain. It is imperative to consider the other causes of right heart strain when evaluating your patient with this ECG finding. Left heart failure is one common cause of right heart strain. Underlying pulmonary pathology, such as pulmonary embolism, pulmonary hypertension, pneumonia, and COPD can lead to right heart strain as well. Intrinsic myocardial disease should not be forgotten as a cause, including ischemia and infiltrative diseases. Valvular and congenital diseases can also lead to this pathology. As in our patient, impaired filling can lead to right heart strain. The patient’s hemorrhagic shock caused a severely low preload and impaired filling which in turn led to the right heart strain as evidenced by the ECG and echocardiogram findings. The resolution of the S1Q3T3 pattern after appropriate volume resuscitation confirms the pathophysiology of this patient’s right heart strain.
Conclusions: The S1Q3T3 sign is a rare but gripping finding in the hospital. It is described as an S wave in lead I, and Q wave with inverted T wave in lead III. However, when it is observed we often associate it only with a pulmonary embolism instead of the overarching cause: right heart strain. It is important to always remember the extensive differential right heart strain includes, as this misconception can lead to misdiagnosis and unnecessary testing. This case highlights the importance of correctly interpreting the S1Q3T3 sign and its association with right heart strain secondary to impaired filling from hemorrhagic shock.