Background: Delirium is an acute, fluctuating confusional state that commonly develops in older and acutely ill hospitalized patients. This condition contributes to patient morbidity and mortality and substantial financial burden to the healthcare system through prolonged hospitalization and increased resource utilization. Clinical decision support within the electronic medical record (EMR) has shown potential to improve adherence to evidence-based practices and decrease physician practice variation. Our objective was to develop and pilot test EMR-embedded clinical decision support using a point-of-care alert to identify patients at high risk of delirium and an order set to encourage high-value delirium management practices.
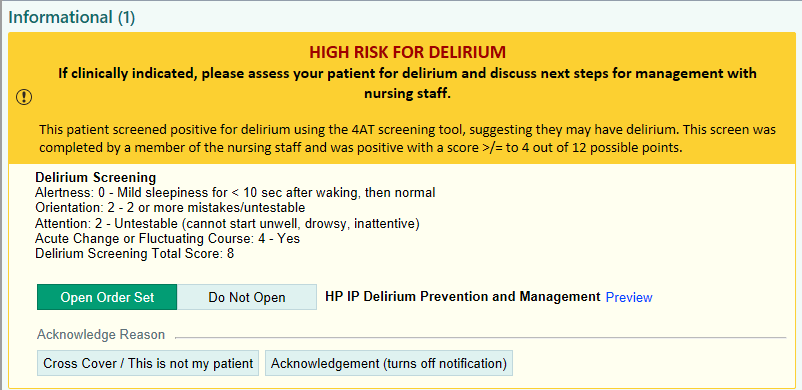
Methods: Our institution had previously implemented universal nursing-led delirium screening using the 4A’s test (4AT), with results entered in the EMR. Our team created a Best Practice Advisory (BPA) within the Epic EMR to alert hospitalists to patients at high risk for delirium (Figure 1). The BPA is activated after a positive 4AT delirium screening score. The BPA provides one-click options to access a delirium management order set or deactivate the BPA. Order set content was determined through literature review (1,2) and feedback solicited from our institution’s multidisciplinary Delirium Taskforce (Figure 2). Notable order set features include a pre-selected high-value management bundle (e.g., frequent re-orientation) and intentional exclusion of restraint orders from the order set. This initiative was pilot tested in a 160-bed general medicine unit within a large Midwestern academic medical center. The BPA and order set were introduced to hospitalists at a section-wide meeting and then implemented on January 24, 2024, with data collected for 6 weeks before and 22 weeks after implementation. Patient inclusion criteria were age 65 or older and a 4AT score of at least 4. Process measures of interest included any restraint utilization (including mitts), antipsychotic and benzodiazepine utilization, and standing bowel regimen.
Results: Number of hospitalizations analyzed was 150 in the pre-intervention period and 323 in the intervention period. Patient characteristics were similar between groups, including average age (78.3 versus 79.6 years), sex (59.3% versus 62.4% female), and peak 4AT score (6.7 versus 6.0 points). There was a significant decrease in restraint utilization between the pre-intervention and intervention periods (32.7% vs 22.0%, p=0.014). There was no statistically significant difference in encounters with at least one antipsychotic or benzodiazepine order (24.7% vs 26.7%, p=0.64) or standing bowel regimen orders (46.0% vs. 45.3%, p=0.89). Forty percent (n=128) of BPA activations resulted in providers placing new orders through the order set.
Conclusions: Implementation of clinical decision support for delirium awareness and management was associated with an 11% decrease in restraint utilization among patients at high risk for delirium during a five month pilot testing period. Notable features of our approach include targeted BPA activation for patients with a positive delirium screen and emphasis of high-value orders such as frequent patient re-orientation. Efforts are underway to implement this clinical decision support system for our institution’s surgical and subpsecialty services.