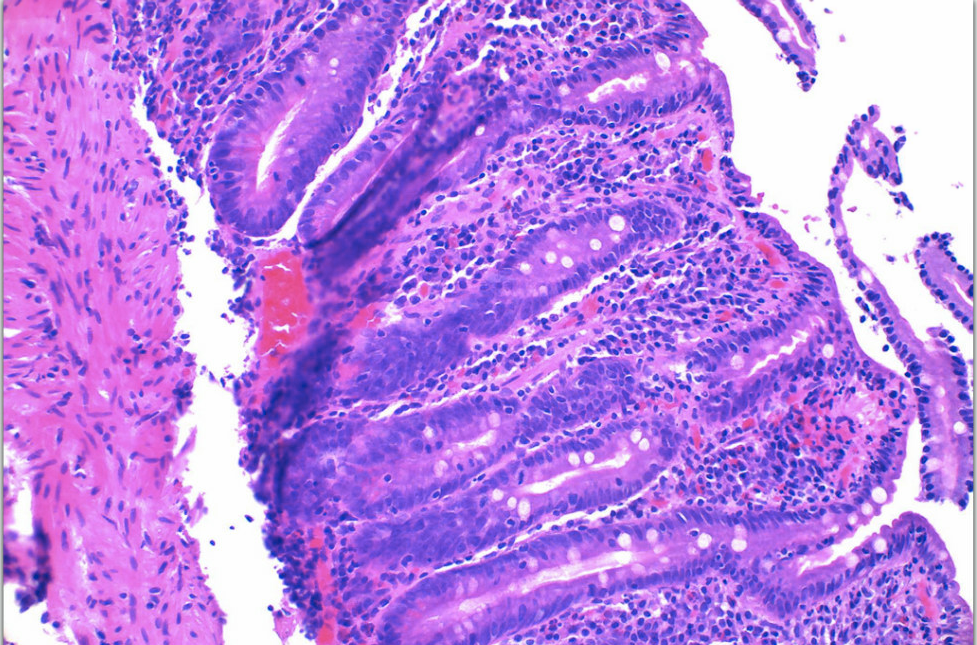
Case Presentation: The patient is a 66-year-old female with a pertinent past medical history of Deep Vein Thrombosis on Eliquis, Hyperlipidemia, Osteopenia, Generalized Anxiety Disorder, Major Depressive Disorder, and Hypertension who presented with a chief complaint of persistent generalized abdominal pain, nausea, vomiting, and watery diarrhea. This was the patient’s fourth admission to the hospital within a three-month period with the same chief complaint. Medication reconciliation performed on admission showed no recent medication changes, with Olmesartan first being prescribed by the patient’s primary care physician 16 months prior to her first hospital admission. During every prior hospital admission Olmesartan would be held as it was not on the hospital formulary, the patient would then report resolution of her symptoms, and then be discharged home on the same medications only to return several weeks later with the same complaint. The patient’s symptoms were attributed to chronic gastritis during previous hospitalizations and the patient was advised to follow up with gastroenterology outpatient, but during this fourth hospital admission the decision was made to proceed with inpatient EGD & Colonoscopy. The only abnormal finding on EGD was non-erosive gastritis within the stomach fundus. Duodenal tissue biopsy showed intraepithelial lymphocytosis, acute inflammation, and crypt apoptosis/villous blunting suggestive of celiac disease, but celiac sprue serology was negative. Histological findings were referred to tertiary care center pathology lab for further study. Upon further evaluation it was noted that the pattern of inflammation and tissue destruction observed throughout the gastrointestinal tract was more consistent with enteropathy induced by angiotensin receptor blocking medications. The patient clinically improved while admitted to the hospital and was discharged on proton pump inhibitor as well as a budesonide taper with instructions to follow up with gastroenterology outpatient. The patient reported complete resolution of her symptoms after completion of budesonide taper, and her symptoms have not returned in over 2 years since discontinuing Olmesartan.
Discussion: Medication induced enteropathy is a medication side effect that was only associated with immunosuppressive drugs such as mycophenolate and azathioprine until 2012 when the first case series about Olmesartan induced enteropathy was published by the Mayo Clinic (1). All cases within this case series had findings analogous to the patient in this case report. Every intestinal biopsy showed villous atrophy and mucosal inflammation, celiac serologies were all negative, and there was no improvement in symptoms with a gluten free diet. Repeat biopsies of all cases in the case series showed evidence of significant histologic recovery with patients reporting complete resolution of symptoms after discontinuing the medication. The mechanism behind this association continues to remain unclear, but the observed delay between initiation of therapy and development of enteropathy symptoms suggests a cell mediated immune response causing tissue damage as opposed to a hypersensitivity reaction (1).
Conclusions: This case report highlights a rare adverse effect of a commonly prescribed antihypertensive medication. Further investigation into this association is warranted to better characterize the adverse effects associated with angiotensin receptor blocking medications.