Case Presentation: A 68-year-old male with 6-months history of dark stools, lightheadedness, and fatigue. He was not on blood thinners. He had three ED visits, two hospitalizations and several office visits and received seven units of packed red blood cells (PRBC) during that time for iron deficiency anemia. Extensive workup with upper GI endoscopy (EGD) & biopsy, two colonoscopies, capsule endoscopy and push enteroscopy were negative. CT enterography during previous admission showed small intraluminal contrast in descending colon; recommended follow-up NM scan was deferred by the gastroenterologist due to suspected false positive result. In this admission, hemoglobin was 5.9, patient received three units of PRBCs. Repeat EGD revealed normal esophageal and gastric mucosa. Hemoglobin continued dropping requiring 5 additional units of PRBCs. Bleeding scan showed active GI bleeding in left mid- abdomen likely in the small bowel. Meckel’s scan was negative for Meckel’s diverticulum. General surgeon performed a diagnostic laparoscopy with resection of 4-inch section of jejunum containing a hyper vascular tumor. Biopsy was positive for low-grade gastrointestinal stromal tumor (GIST), spindle cell type.
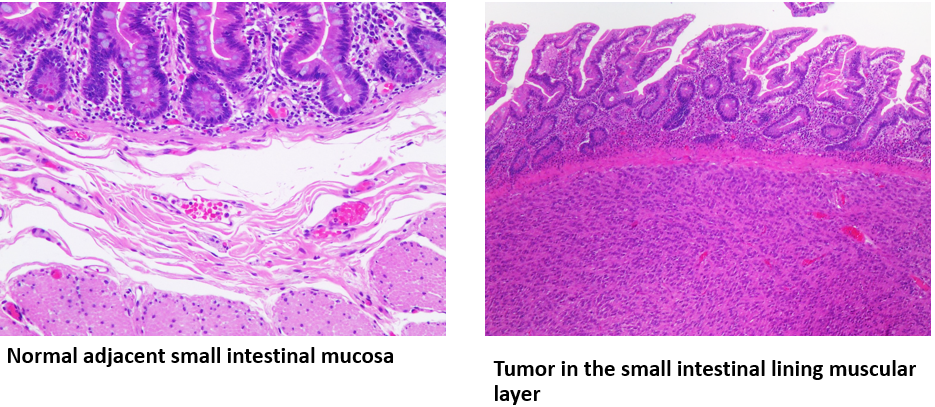
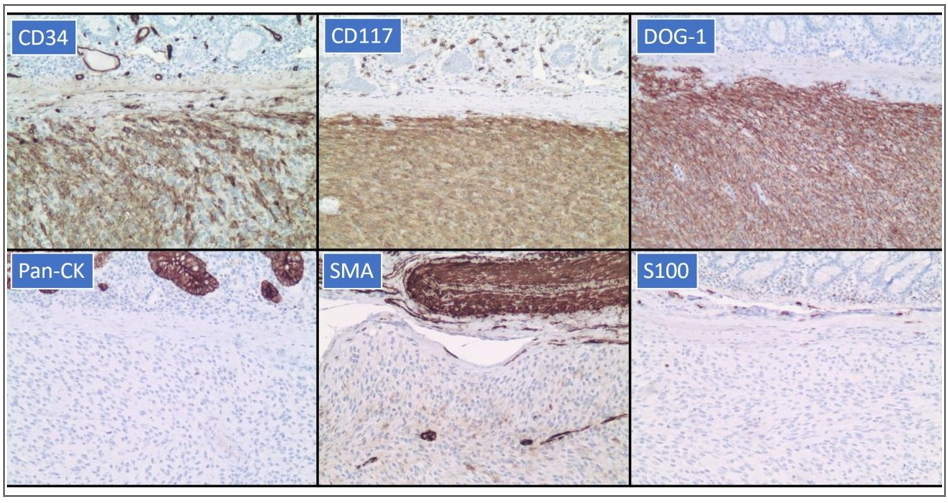
Discussion: GISTs are the most common mesenchymal neoplasms of the GI tract, they can nevertheless be missed with commonly used diagnostic modalities like EGD with mucosal biopsy done for most cases of GI bleed. Mucosal biopsies would typically show reactive changes and miss the tumor since GISTs arise from the interstitial cells of Cajal located in the intestinal wall muscular layer. In this patient, persistently negative workup with small intestinal location of bleed made a laparoscopic approach necessary. Fortunately, the resected portion contained the tumor, effectively diagnosing and treating simultaneously; this patient’s hemoglobin has remained stable months after the tumor resection.
Conclusions: Obscure GI bleed is often difficult to diagnose and all techniques including the new and older diagnostic modalities should be incorporated to save time and reduce mortality. In cases of GI bleed with unrevealing workup, less common etiologies should be considered, and invasive techniques may be necessary to reach a definitive diagnosis.