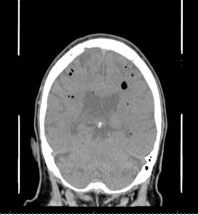
Case Presentation: A 75-year-old male with a past medical history significant for coronary artery disease, paroxysmal atrial fibrillation on Eliquis, hypertension, and hyperlipidemia presented to the emergency room with complaints of left-sided weakness, more pronounced in the left upper extremity. Physical examination revealed an alert, oriented, and well-appearing gentleman with decreased strength in his left upper and lower extremities and a left-sided facial droop. Lungs were clear to auscultation, and cardiac examination showed a regular rate and rhythm with a grade 1/6 systolic ejection murmur. A CT brain attack demonstrated bilateral cortical infarcts. TPA was contraindicated due to recent Eliquis use, and he was admitted for further management. On the second day of admission, the patient became obtunded, prompting a rescue alert. He was intubated for airway protection, and a subsequent CT brain scan showed similar findings as before but now with marked pneumocephalus. The patient was transferred to the ICU and remained on mechanical ventilation with 100% FiO2. An echocardiogram with a bubble study revealed a large, echogenic, irregular, mobile thrombus in the superior cavity of the left atrium. A CT pulmonary embolism study showed a filling defect in the left atrium consistent with thrombus and associated gas within the thrombus. All four blood cultures drawn were positive for Streptococcus Salivarius and Mitis.
Discussion: A gas-containing left atrial thrombus presents a significant risk for complications. The thrombus itself may dislodge from the atria, travel through the arterial system, and result in acute infarcts. When the thrombus contains gas, the gas can be released into the surrounding brain tissue, leading to pneumocephalus. The presence of gas within the thrombus may arise from various factors. One possibility is an infected thrombus with a gas-producing organism. S. Salivarius, which was the bacteria identified in this patient can lead to gas formation. It has a unique urease system in which urea is broken down to release gases such as Ammonia and CO2 [1]. Another potential cause is the iatrogenic introduction of air into the venous system, with bubbles large enough to travel across the pulmonary bed to the left atrium. However, at the time of decompensation, the patient had only two peripheral IV accesses and had not undergone any invasive procedures.
Conclusions: The etiology of gas-containing left atrial thrombus remains uncertain, and further investigation is needed to determine the underlying cause. Regardless of the source, prompt recognition and management of such a thrombus are crucial to minimize the risk of severe neurological complications and improve patient outcomes.