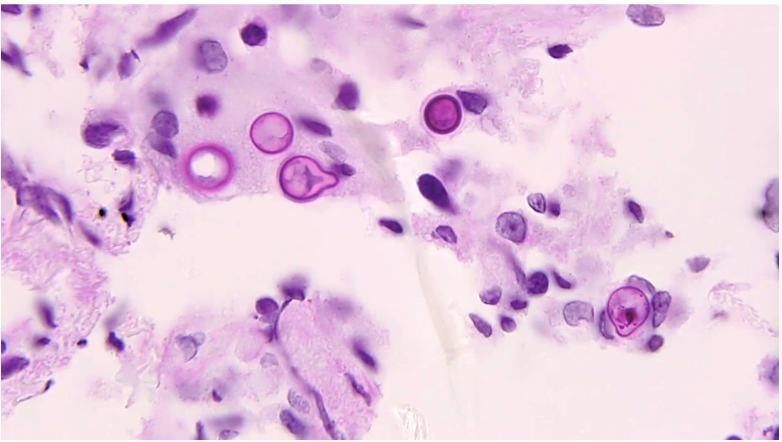
Case Presentation: A 38 yo male with PMH of alcohol abuse, motor vehicle collision a year prior to presentation, presented to the ED with back pain. Pt states that had back pain about a year ago right after the motor vehicle collision, which improved after a month. Then in the last 4 weeks, he has been getting significant acute severe low back pain. He had a CT completed as an outpatient that showed a burst L5 compression fracture and followed up with neurosurgery – plan was for conservative management.On presentation, pt had stable vitals, leukocytosis of 16.3 with left shift, ESR 150, and CRP of 113. Infectious disease (ID) was consulted given leukocytosis, as well as pain service and neurosurgery team. An MRI was obtained and it redemonstrated the burst L5 fracture (figure 1). Etiology of burst compression fracture was unclear – ID felt this was less likely infectious. Per discussion with the radiologist, there was concern about the findings to be due to malignancy. Oncology was also then consulted – and a CT chest was ordered as well. This showed multiple micronodules. The consensus was to obtain a biopsy, which was completed on day 2 of admission. Meanwhile the pain team continued to adjust medications to help him with his severe pain. On day 4, the patient started spiking fevers with temperature up to 103, and was noted to have worsening leukocytosis. Pathology was contacted for preliminary results given worsening clinical status – and they noted fungus on the slides, consistent with blastomycosis (figure 2). The patient was finally started on appropriate therapy with itraconazole and clinically improved, and was eventually discharged in stable condition.
Discussion: The incubation period of disseminated blastomycosis is highly variable. Extrapulmonary manifestations that are typically in the skin, GU system, and bones – often due to hematogenous spread from a pulmonary source. The skin lesions are the most common and present as verrucous lesions and subcutaneous nodules. The second most common extrapulmonary manifestation of disseminated blastomycosis is bone lesions. Typically, disseminated blastomycosis presents as osteomyelitis of the vertebrae, pelvis, and sacrum. Specifically in the vertebrae, disseminated blastomycosis can present with anterior involvement of the vertebral body and destruction of the disc interspace, similar to tuberculosis. This patient’s presentation was unique in that he presented with a burst fracture – which is not typically associated with blastomycosis. An L5 burst fracture is typically due to fall or MVA and rarely associated with an infection. The pathophysiology includes a strong force that pushes the nucleus pulposus into the intervertebral disc causing the vertebral body to shatter outwards. This unique case demonstrates a rare situation where an L5 burst fracture is caused by an infectious etiology rather than traumatic. In order to maintain a high index of suspicion, it is important to be aware of these atypical presentations.
Conclusions: Back pain can be caused by numerous etiology. This case illustrated an interesting case of a burst fracture due to blastomycosis, with no other symptoms until later in the hospitalization (including no pulmonary symptoms) in an immunocompetent patient. A bone biopsy was appropriately pursued to aid in the diagnosis.