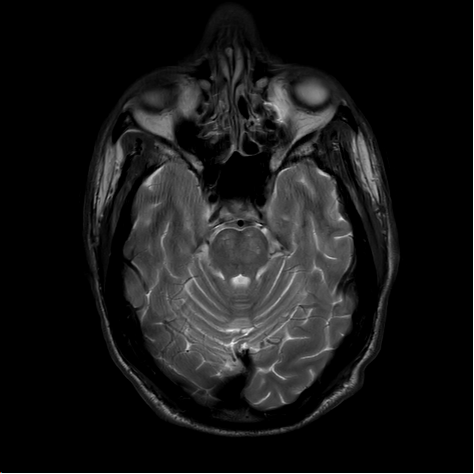
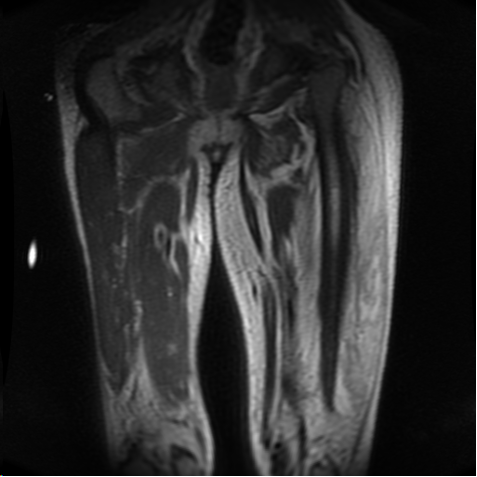
Case Presentation: A 44-year-old man with a past medical history of poorly controlled diabetes mellitus type 2 presented to the emergency room with 7 months of bilateral leg pain and swelling that acutely worsened in the last 2 weeks and multiple recent mechanical falls. The falls were not associated with loss of consciousness or other prodromal symptoms. He also noted new onset dysarthria for the prior month. Physical exam revealed normal vitals, mild non-pitting edema of the lower extremities (left greater than right), hyperpigmented skin lesions on the anterior lower extremities, and tenderness to palpation of the left hip and knee. On neurologic exam, he had 3/5 and 4/5 strength in the left and right lower extremities, respectively, hyporeflexia, dysmetria, and decreased proprioception and vibration sense bilaterally, and occasional stuttering with slurred speech. He also noted dysphagia with solid foods. Labs were remarkable for a WBC of 16.6 103/ul with neutrophilic predominance, hemoglobin of 9.6 gm/dL, glucose of 433 mg/dl, and HbA1C of 12.2. Chest x-ray, EKG, Doppler ultrasound of the lower extremities, TTE, and CT head showed no abnormalities. MRI Brain/Spine demonstrated abnormal restricted diffusion and T2 flair hyperintensity in the bilateral pons consistent with osmotic demyelination syndrome (ODS). Further workup for the patient’s left leg erythema and pain revealed creatinine kinase of, CRP 191 mg/L, ESR of 120 mm/Hr, and Aldolase of 8.5 u/L. MRI of the left femur showed diffuse changes in the anterior extensor compartment of the thigh concerning for diabetic myonecrosis. Treatment for our patient’s diabetic complications involved optimal glucose control, aspirin for diabetic myonecrosis, and discharge to a rehabilitation facility for physical and occupational therapy.
Discussion: Our patient presented with two rare complications of diabetes, osmotic demyelination syndrome (ODS) and diabetic myonecrosis, and there are no prior reports from our literature search of these conditions co-occurring. ODS results from rapid osmolar shifts and leads to cerebral edema. While sodium is the most common causative osmole, there are prior case reports of glucose shifts alone leading to ODS. Given that our patient’s sodium was stable, neurology and endocrinology concluded that frequent fluctuations in blood glucose (range 100-500) led to ODS and accounted for the symptoms of dysarthria and dysphagia. The pathophysiology of diabetic myonecrosis is poorly understood but presents as acute or sub-acute swelling and pain of a lower extremity in patients with microvascular complications of diabetes. Inflammatory markers are often elevated and the condition is best diagnosed with MRI imaging. In our patient, diabetic myonecrosis in addition to diabetic polyneuropathy contributed to his falls. Treatment involved aspirin, glucose control, and rehabilitation therapy.
Conclusions: For hospitalists, this case underlines the importance of maintaining a broad differential and recognizing rare complications such as ODS and diabetic myonecrosis when approaching a patient with poorly controlled diabetes and unexplained neurologic symptoms. Furthermore, this case highlights the importance of ensuring adequate glucose control for hospitalized patients and ensuring proper transition of care to an outpatient care team to prevent such complications.