Background: Many hospitalized adults arrive with pre-existing malnutrition, which is associated with high risk of adverse outcomes. As such, malnutrition is a common variable in cost and quality risk adjustment models based on hospital discharge diagnosis codes. Hospital dietitians assess patients for malnutrition and generally document the details of their evaluations. However, coding professionals cannot assign diagnosis codes from dietitians’ notes but must rely on the documentation of inpatient providers who generally confirm the diagnosis and order appropriate treatments but often fail to include sufficient details in their notes to support coding. Similar to other hospitals, documentation specialists in our hospital query providers to include more details when notes are lacking. Herein we report the effect of a novel, electronic medical record (EMR) tool to reduce malnutrition documentation queries by automatically importing details, in discrete data fields, from dietitians’ notes into providers’ draft progress notes and discharge summaries.
Methods: When providers create or copy-forward a note, the tool looks retrospectively to import dietitian note details about malnutrition, when present. After piloting and refining the tool, we asked inpatient internal medicine providers in our hospital to add it to their note templates. To assess the effect on queries, we observed 200 consecutive internal medicine discharges prior to the intervention and 200 consecutive discharges following the intervention, all with dietitian-determined malnutrition. We examined two primary outcomes: the presence of a malnutrition documentation query and the presence of a malnutrition discharge diagnosis code.
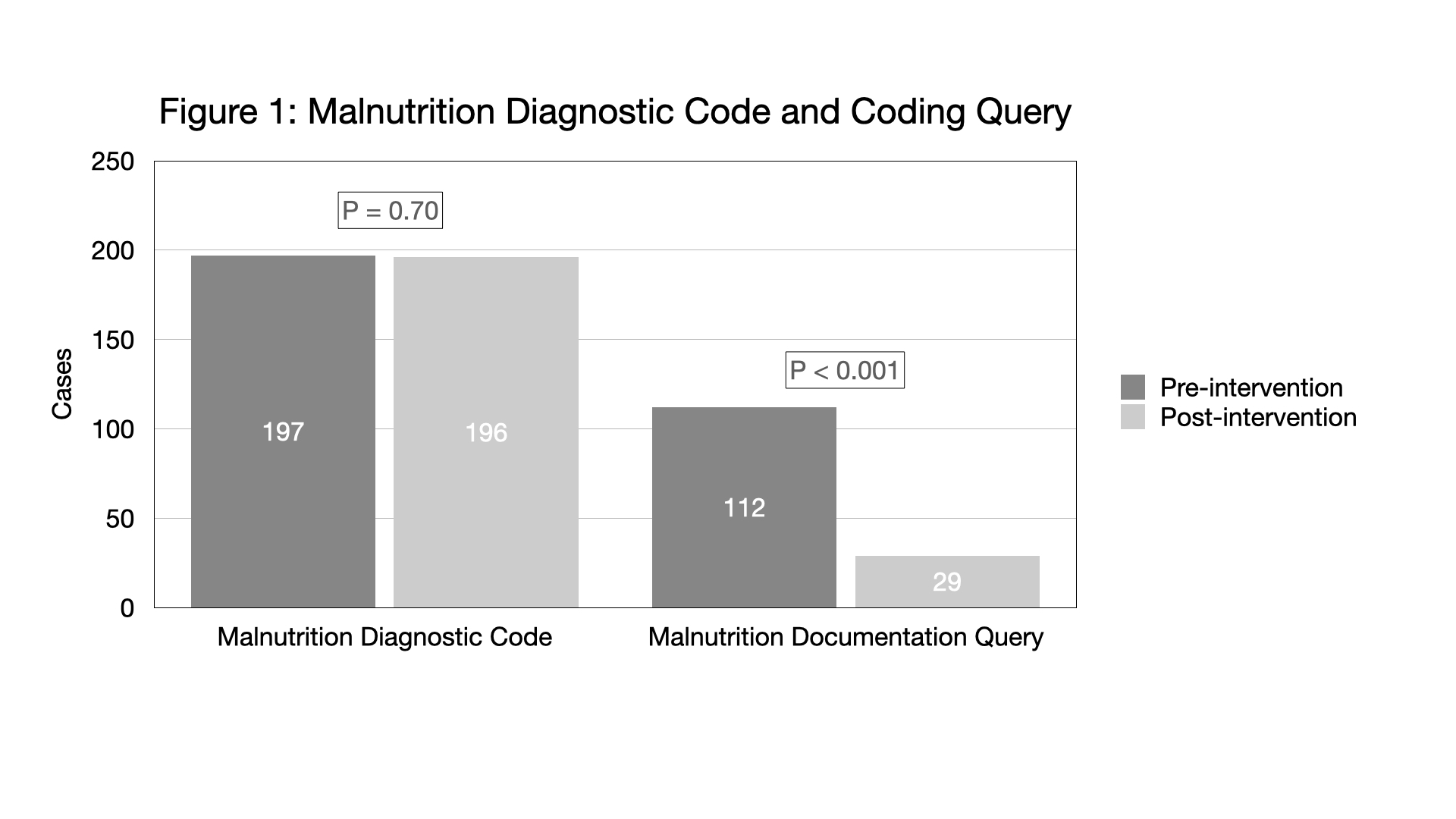
Results: Among the 400 total discharges, the median age was 62 (interquartile range 48-72) years. The cohort was 56% male, 54% African American, 37% White, 3% Asian, and 6% Multi-racial or other. Of the 200 pre-intervention discharges, 112 (56%) received documentation queries, and 197 (99%) received a malnutrition diagnosis code (figure 1). Of the 200 post-intervention discharges, 29 (15%, p< 0.001 vs. pre-intervention) received documentation queries and 196 (98%, p=0.70 vs. pre-intervention) received a malnutrition diagnosis code (figure 1). Of the 29 post-intervention discharges that received a malnutrition documentation query, in 27 (93%) the provider had not adopted the tool into their progress note, in one case the dietitian documentation deviated from the documentation protocol, and in the final case a query was sent despite use of the tool with sufficient documentation.
Conclusions: Introduction of this tool decreased the need for clinical documentation coding queries by nearly three quarters without compromising discharge diagnosis coding. Over 90% of the queries sent during the post-intervention time period were for cases where the providers had not adopted the tool into their note template. This EMR tool provides a model which might be extrapolated to optimize documentation of other conditions by importing discrete data into draft notes in order to help providers document details needed for accurate coding.