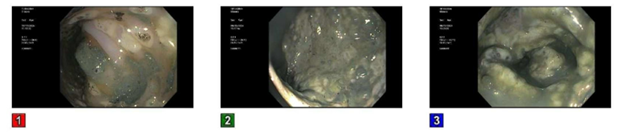
Case Presentation: A 63-year-old female with a past medical history of stage III breast cancer status post double mastectomy in 2017 with bilateral implants presented to the emergency department for left breast implant rupture and dehiscence. She was started on broad spectrum antibiotics with Vancomycin and Zosyn and was later switched to Meropenem. Chest CT with contrast revealed bone metastases and the patient was diagnosed with Stage IV recurrent ER(+) breast cancer. She was started on hormone-based chemotherapy with Letrozole. She underwent debridement of bilateral chest wounds with application of split thickness skin graft and wound vac to the chest wall skin graft. The patient was to continue Meropenem until grafting was successful. However, on twentieth day of hospitalization patient was noted to be lethargic but still able to follow commands. Abdomen was significantly distended, tympanic, and tender. Per nursing staff patient had been constipated for days. Lactic acid was normal. Computed tomography image of abdomen and pelvis without contrast revealed colon severely dilated to a diameter of 9.05 cm. C. difficile PCR as well as C. difficile Toxin Immunoassay was found to be positive. Patient was on Meropenem for twenty days so that was discontinued. She then underwent flexible sigmoidoscopy and decompression by GI. Rectal tube was left in place. Patient was noted to have several episodes of liquid dark brown diarrhea after that. She was then started on Vancomycin enema and IV Flagyl and eventually converted to PO Dificid when her acute toxic metabolic encephalopathy resolved and she was able to swallow. She was eventually discharged in stable condition and will follow up outpatient with Hematology/Oncology regarding her breast cancer treatment.
Discussion: Pseudomembranous colitis is a severe inflammation of the large intestine that is often caused by a Clostridium difficile infection (CDI). It is important to know the risk factors of CDI as our patient did not present with the classic presentation of frequent bowel movements for several days or diarrhea. In fact she was constipated. However, knowing that she had been on Meropenem for twenty days honed us to the diagnosis. The risk factors for CDI are: advanced age (persons > 65 years), inflammatory bowel diseases (IBD), human immunodeficiency virus infection, hematologic malignancies, chronic kidney disease, increased duration of hospitalization, exposure to antibiotics/chemotherapeutic agents, and the use of proton pump inhibitors and upper gastro-intestinal tract surgery. It is important to note that she was also started on Letrozole for her Stage IV breast cancer, another risk factor. Patient improved with conservative management (decompression via flexible sigmoidoscopy and rectal tube) and IV Flagyl and Vancomycin enema that was later switched to PO Dificid. Luckily, she did not need a colectomy. Please note our patient did not meet the diagnostic criteria for toxic megacolon.
Conclusions: It is important for physicians to recognize pseudomembranous colitis early on due to the increased mortality that occurs in cases associated with colonic perforation, peritonitis, septic shock and multiple organ dysfunction. Early diagnosis and treatment of pseudomembranous colitis is crucial.