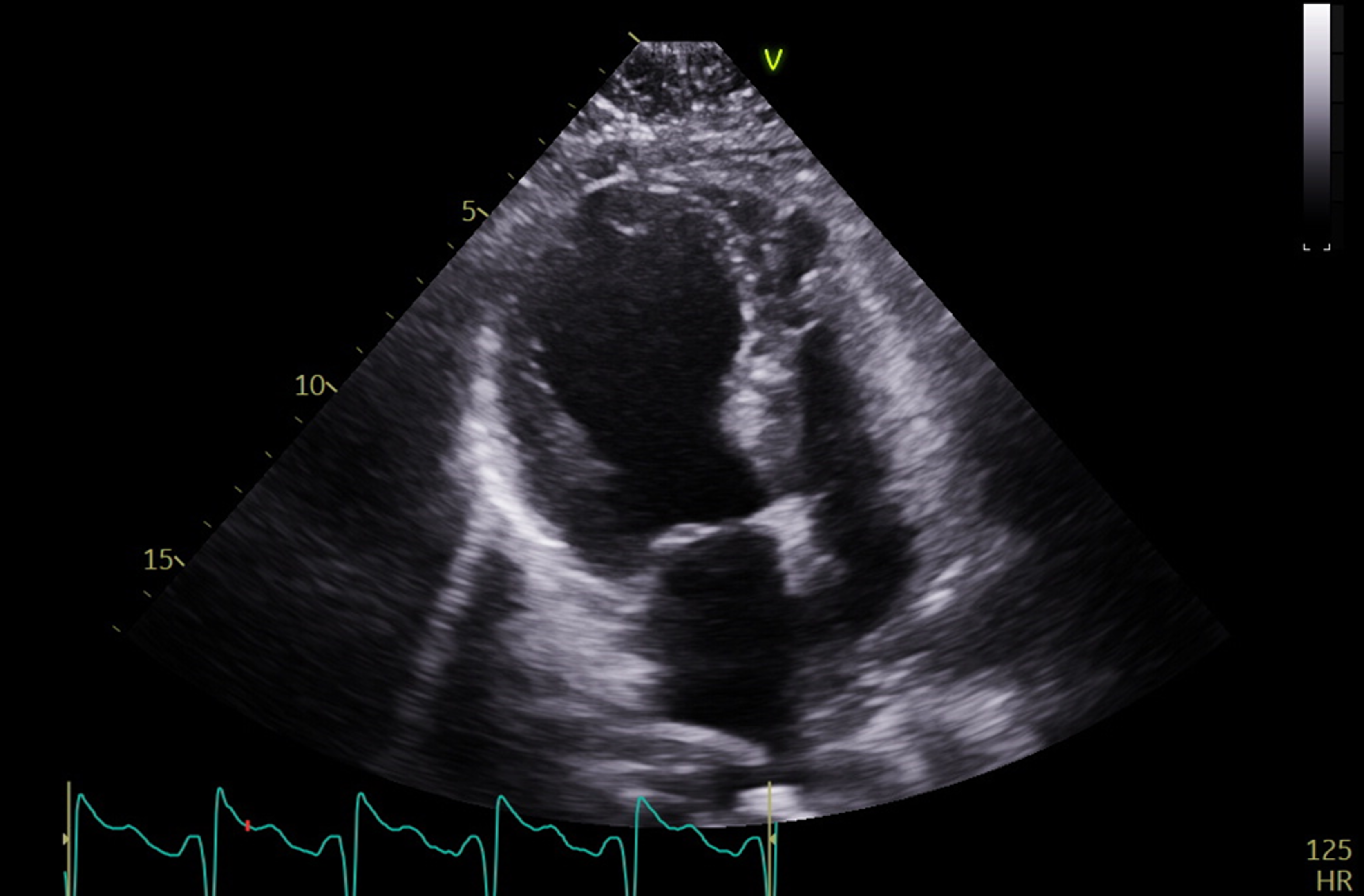
Case Presentation: A 60-year-old female with poorly controlled type 2 diabetes mellitus (A1c 11.8%) on insulin and previous stress cardiomyopathy during an episode of DKA with subsequently recovered systolic function presented with chest pain, nausea and vomiting following four days of cough and sore throat. On arrival, laboratory findings included: glucose 634 mg/dL, beta hydroxybutyrate 3.0 mmol/L, pH 7.29, and anion gap 21; this was concerning for DKA and intravenous fluids and insulin infusion were started. CT scan of the chest demonstrated atypical multifocal pneumonia for which she was started on broad spectrum antibiotics. Initial EKG showed no acute ischemic changes. Baseline high sensitivity troponin was 65 which increased to 494 ng/L at two hours and she was subsequently transferred to the cardiac ICU for further management. On arrival to the ICU, despite improved glycemic status and stable hemodynamics, her lactate increased to 5.3 mmol/L. On physical examination, her extremities were cold, and she was tachypneic with evidence of pulmonary edema and reduced left ventricular systolic function on bedside ultrasound. Blood pressure was normal, so diuresis was initiated and she was started on nitroprusside and milrinone guided by a pulmonary artery catheter. Echocardiography confirmed a decreased left ventricular ejection fraction of 32% with apical akinesis and preserved function at the basal levels suggestive of stress cardiomyopathy. The patient had a recent prior coronary angiogram which showed no significant coronary artery disease. Over the following days, the patient’s DKA resolved, and her respiratory status improved with diuresis and antibiotic therapy. She was gradually transitioned from intravenous vasoactive medications to guideline-directed medical therapy with lisinopril and carvedilol. Repeat echocardiogram prior to discharge demonstrated an improved left ventricular ejection fraction of 52% with improved function at the apex. She was discharged home in stable condition on hospital day number eight.
Discussion: Stress cardiomyopathy, also known as takotsubo cardiomyopathy or apical ballooning syndrome, is characterized by transient regional systolic dysfunction typically involving the left ventricle in the absence of obstructive coronary artery disease. Both emotional triggers as well as physical stress have been associated with development of stress cardiomyopathy, and a recent study involving the International Takotsubo Registry reports rates of 27.7% versus 36.0%, respectively. The underlying etiology is unclear, though the most widely accepted mechanism is due to a catecholamine surge leading to microvascular spasm and myocardial stunning by overactivation of adrenergic receptors. Very few instances of takotsubo cardiomyopathy triggered by DKA have been described previously. Moreover, to our knowledge there have been no documented cases of DKA triggering both the initial diagnosis of stress cardiomyopathy as well as its recurrence. Management is supportive and directed at addressing the underlying precipitant, with guideline-directed medical therapy for systolic heart failure often considered.
Conclusions: This case illustrates the importance of evaluation for stress cardiomyopathy in patients who have evidence of myocardial infarction, heart failure or cardiogenic shock during treatment for DKA in the absence of coronary artery disease. This is particularly important in patients with a history of prior stress cardiomyopathy.