Background: According to the Global Burden of Disease (GBD) study, 523 million (95% UI: 497 to 550 million) people worldwide had cardiovascular diseases (CVDs) in 2019, resulting in a significant increase in DALYs and years of life lost, mostly due to ischemic heart disease. There are various accurate and economical gold standard tests to identify CVDs, but increasing burden-specific requirements necessitate the use of AI and ML. We aimed to identify accuracy of artificial intelligence (AI) and machine learning (ML) in diagnosing CVDs.
Methods: We did a systematic review using the PRISMA protocol and MOOSE guidelines to identify the observational studies and clinical trials that used different types of AI and ML to diagnose CVDs or studies having data on diagnostic accuracy from PubMed in 10 years. Non-original articles, non-English, non-Human, and non-full-length studies were excluded. The data obtained from the studies included information on sensitivity and specificity. We have also collected the data on study name, type, population of interest, sample size, comparison arms, AI or ML model name, and their diagnostic accuracy.
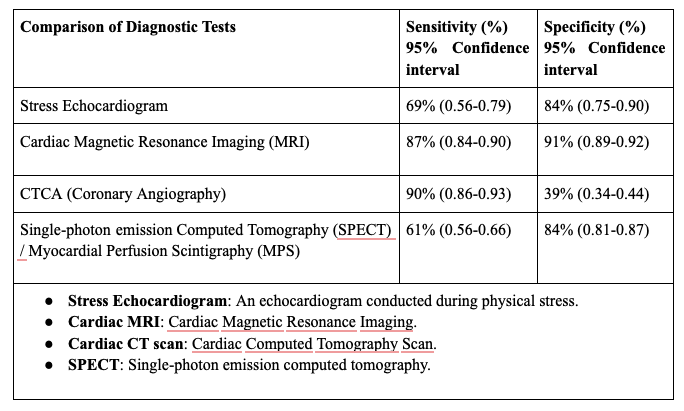
Results: We found 21 studies showing use of AI and ML in diagnosing CVDs. The studies reviewed emphasize the growing role of artificial intelligence (AI) in cardiac MRI imaging. Many studies demonstrate high accuracy in heart segmentation and functional assessment, such as the work by Bernard et al. (2018) and Bai et al. (2018), showing performance comparable to human experts in analyzing cardiac structures. Similarly, Tao et al. (2018) and Wong et al. (2022) highlight the reliability of deep learning in automated heart function analysis, suggesting potential for widespread clinical adoption. AI techniques have also been instrumental in improving image acquisition speed and quality. Studies like Fotaki et al. (2021) and Manuel et al. (2024) illustrate advancements in 3D imaging and reduced scan times, enhancing efficiency in clinical workflows. Moreover, research on specific conditions, such as Zhang et al. (2021) on hypertrophic cardiomyopathy, confirms the promise of AI-driven diagnostic tools in detecting structural abnormalities with minimal reliance on contrast agents. Despite these advancements, challenges persist, including small sample sizes, single-center studies, and limited generalizability, as seen in works like Fuin et al. (2020) and Ghadimi et al. (2021). Future research should address these limitations through larger, diverse datasets and standardized imaging protocols to fully integrate AI into routine cardiac care.
Conclusions: AI and ML are transforming cardiovascular care by enhancing diagnostic accuracy, predicting disease progression, and streamlining clinical workflows. Their applications in ECG, echocardiography, MRI, and CT have shown high sensitivity in detecting conditions like hypertrophic cardiomyopathy and coronary artery disease. Addressing data heterogeneity and improving algorithm integration are critical for optimizing outcomes and reducing the global CVD burden.