Background: Suicide is the second leading cause of death for adolescents age 15-19 in the United States and ingestion/poisoning hospitalizations continue to rise. In order to better understand this population, we investigated characteristics of adolescent poisoning hospitalizations including patient factors as well as ingestion history.
Methods: Retrospective study of adolescent patients (aged 12-18) hospitalized to hospital medicine or critical care service due to acute intoxications or poisoning at a freestanding children’s hospital in the Midwest from January 2019 through December 2019. Patients living in the city zip code were stratified into a lower, middle, or upper socioeconomic status (SES) region based on their zip code.
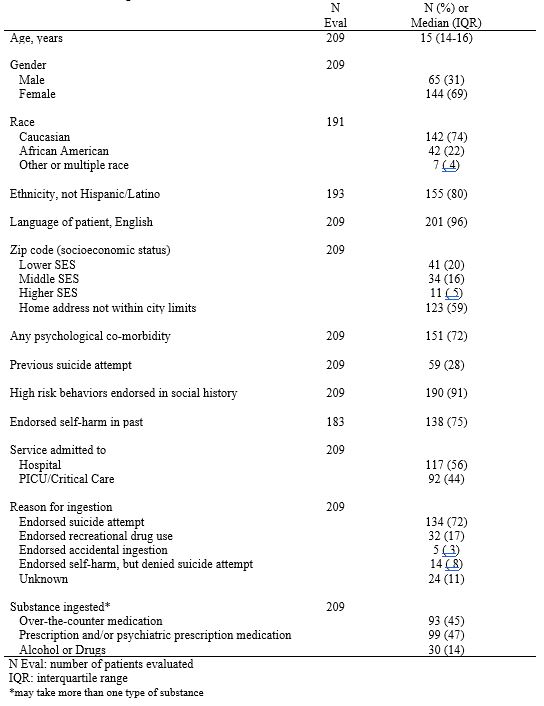
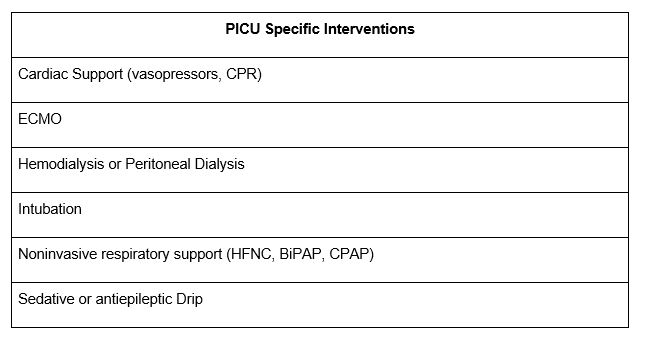
Results: 209 unique encounters were reviewed. Overall patient and ingestion history characteristics are described in Table 1. Median age (interquartile range) of patients was 15 (14-16) years with the majority being female (69%). At least one psychiatric comorbidity was present in 72% of patients. Presence of high risk-behaviors (having had sex, drank alcohol, or used tobacco, any drugs or vaped) was endorsed in 9 out of every 10 patients (91%). Two thirds of patients endorsed previous self-harm and around a quarter endorsed a previous suicide attempt. Of the 86 patients from city zip codes, 87% were from lower-middle SES zip codes while only 13% were from higher SES zip codes. The majority of patients (64%) endorsed a suicide attempt as reason for ingestion. Of all patients, only 14% reported ingesting alcohol, marijuana, or other recreational drugs, illustrating that these substances constitute only a small percentage of adolescent poisoning hospitalizations. A little less than half of patients were placed on the critical care service on admission and four patients were transferred to critical care during their hospitalization. Of the 95 patients who required a pediatric intensive care unit (PICU) stay during their hospitalization, only 16% (15/95) received PICU specific intervention (Table 2).
Conclusions: Specific target populations for preventative interventions include adolescents with a diagnosed psychiatric disorder, from lower-middle SES regions, and those who have endorsed a previous suicide attempt, previous self-harm, or other high-risk behaviors. In addition to evaluating risk for self-harm and encouraging follow up in those adolescents hospitalized due to poisoning, these findings highlight the importance of always assessing for high risk behaviors as they are present in greater than 90% of these encounters. Adolescents with risk factors may benefit from thoughtful and deliberate restriction in access to prescription and over the counter medications at home. Finally, while a little less than half of patients required a PICU stay during their hospitalization, only a minority of adolescents received a PICU specific intervention suggesting further research is needed to potentially optimize patient placement on admission to the hospital.