Background: Joint physician-nurse rounding is an important best practice that facilitates communication and patient participation in their care while improving outcomes and satisfaction. Interdisciplinary bedside rounding has been shown to reduce mortality, lengths of stay, medication errors, and readmissions while improving staff engagement, teamwork, and patient experience (1, 2, 3). In 2018, our hospital added the following question to our Press Ganey HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) survey to measure patients’ perception and impact of joint rounds: “If a doctor and nurse visited you (rounded) together, did it help you to better understand the plan for your care?” Our data show that units with higher percentages of patients answering “Yes” to this question perform higher in overall hospital rating, likeliness to recommend, and HCAHPS domains including communication with nurses and doctors and about medications, responsiveness, hospital environment, discharge information, and care transitions. However, we had limited ability to track process metrics and identify and overcome barriers.
Purpose: To improve joint physician-nurse rounding, we developed a custom dashboard to track joint rounding occurrence. Providing transparent data establishes accountability and ownership and allows for leaders and stakeholders to better understand trends.
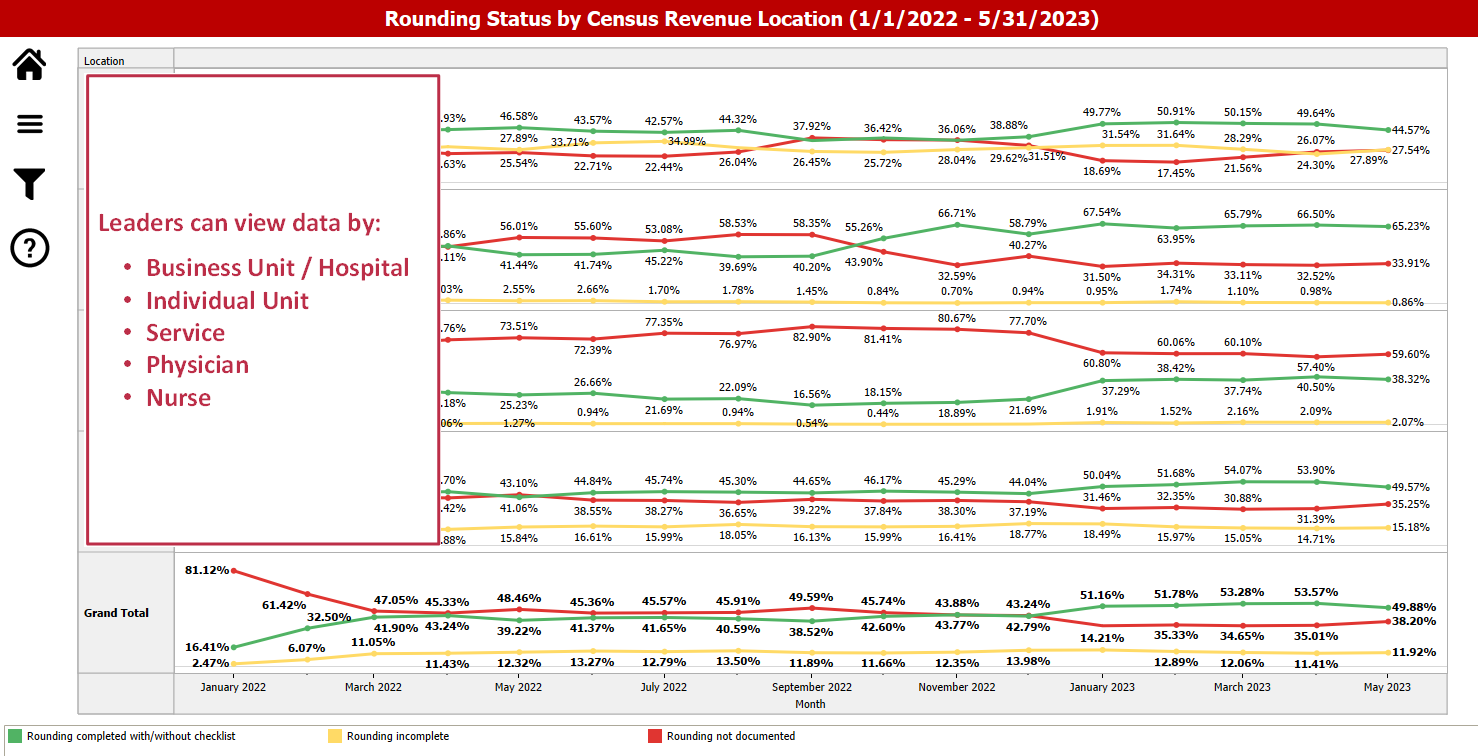
Description: Data is gathered into the dashboard from the Epic/IHIS electronic medical record. Nurses document rounds in the patient FLOWSHEET. Entries are queried to determine if rounding has occurred, not occurred, or if nothing was documented each day. A determination is also made as to which physician and nurse are responsible for rounding based on those assigned to the patient’s TREATMENT TEAM each morning. The dashboard displays percentages of joint rounds as completed, not completed, or if nothing was documented. These data are presented for each clinical unit and service, as well as for specific physicians and nurses.This has added a new level of accountability, allowing unit and service level leaders to focus efforts. We are now able to assess if joint rounds are occurring or not, and if there are issues with the physician, nurse, or patient’s perception by comparing dashboard data to the Press Ganey survey data. When we implemented the dashboard in FY22, joint rounding was being documented as occurring only 15% of the time. By April 2022, we saw that increase to 47% and maintain that for remainder of FY22. Late FY22 into early FY23 we saw a plateau in joint rounding documentation. By reviewing the unit-by-unit data, we identified high performers and derived best practices to leverage them on lower performers. Using these strategies, we have started seeing an increase in joint rounding. We were able to begin correlating the impact of joint rounding on key HCAHPS domains. We saw the greatest improvements in our Doctor Communication (from the 42nd to 67th percentile), Communication about Medications (from the 35th to 74th percentile), and Nurse Communication (from the 48th to 64th percentile). In addition, we identified that when joint rounding occurs, our likeliness to recommend score increases to the 86th percentile.
Conclusions: The development of this dashboard is uniquely innovative as it is a new method to track interdisciplinary rounding from the patient electronic medical record. We can leverage this data to identify barriers and add accountability to improve joint physician-nurse rounding.