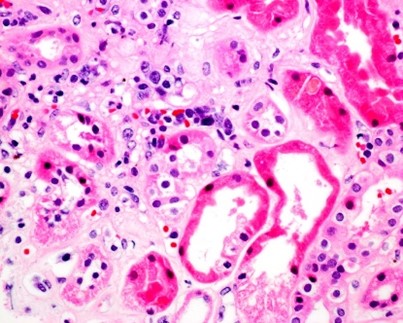
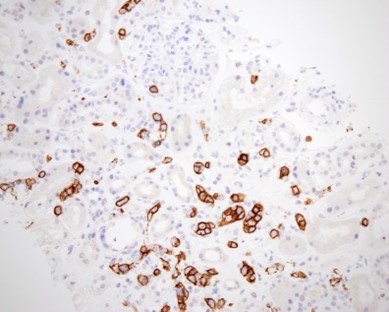
Case Presentation: A 74-year-old female with a history of restless leg syndrome, hypertension, GERD, presented with worsening fatigue, shortness of breath, and anasarca over the last 6 months. Labs revealed anemia (hemoglobin, 8.0 g/dL), thrombocytopenia (platelet count, 46K/μL), reticulocyte count 11.4%, undetectable serum haptoglobin, serum LDH >2700 U/L, ferritin 1223 ng/mL, negative direct Coomb’s test, BUN 92 mg/dL, serum creatinine 1.60 mg/dL, AST 155 U/L, ALT 13 U/L, and elevated total bilirubin 5.2 mg/dL. As such workup was consistent with nonimmune hemolytic anemia. Serum fibrinogen, factor 8, SPEP, and ADAMTS13 were normal. HIV, hepatitis B, and C viral markers were negative. A peripheral smear showed no schistocytes. Bone marrow biopsy did not show any immunophenotypic evidence of a lymphoproliferative disorder, acute leukemia, plasma cell neoplasm, or hemophagocytic lymphohistiocytosis. Flow cytometry, cytogenetics, FISH, and molecular panel were normal. CT scan showed an enlarged anterior mediastinal lymph node of 2.6X1.9 cm, splenomegaly (16.2X8.3X6.5cm), diffuse anasarca, bilateral axillary lymphadenopathy, and normal liver. The patient was eventually found to have nephrotic range proteinuria (6 g/day and urine protein-to-creatinine ratio of 6.05). A renal biopsy revealed intravascular B cell lymphoma (ILBL), and most of the glomeruli infiltrated with atypical large lymphoid cells in the capillary lumina (Fig A), and no evidence of thrombotic microangiopathy. Immunohistochemical stains demonstrated strong CD20 (Fig B). The diagnosis of renal ILBL was confirmed. Thereafter, patient and family chose to transition to inpatient hospice and comfort measures.
Discussion: ILBL is a rare subtype of Large Cell Lymphoma with varied clinical presentation and poor prognosis (1). It is characterized by the growth of lymphoma cells in the lumen of blood vessels without a discernible tumor mass and the absence of circulating neoplastic cells in the peripheral blood in more than 90% of cases (1). The median age of diagnosis for ILBL is 70 years with no gender predisposition. Clinical presentation is nonspecific and heterogeneous. The spectrum of symptoms depends on the organ system involved (1). Fever of unknown origin is the most common symptom in about 50% of the patients. Laboratory findings can also be nonspecific including anemia, leukopenia, thrombocytopenia, elevated ESR, and tests showing liver, kidney, and thyroid dysfunction. The large neoplastic cells of ILBL have a high nuclear-cytoplasmic ratio and display the immunophenotype of mature B cells with strong CD20 expression (1). Cytogenetic studies demonstrate clonal rearrangements of immunoglobulin genes in malignant cells. Renal involvement of ILBL is infrequent and there are only a couple of case reports of it presenting as Nephrotic Syndrome (2). ILBL and its infrequent presentations need a high index of suspicion for diagnosis and a definitive diagnosis needs a histopathological examination of the biopsy specimen. The biopsy location depends on the organ system involved, kidney in this case. ILBL is an aggressive disease and needs prompt treatment with a combination of cyclophosphamide, doxorubicin, vincristine, and prednisone with the recombinant anti-CD20 antibody rituximab (R-CHOP).
Conclusions: Nephrotic Syndrome is an unlikely and unusual presentation of Intravascular large B cell lymphoma (ILBL). It is important for hospitalists to have a high index of clinical suspicion to avoid delayed diagnosis and treatment.