Background: Medication reconciliation is a complex process intended to identify and resolve discrepancies by maintaining the most accurate medication list for a patient to provide ultimate care. The Joint Commission National Patient Safety Goals emphasize completion of medication reconciliation on admission within an organization to reduce the likelihood of harm to patients.1 Our medical center set a goal of admission medication reconciliation compliance (AMRC) rate above 90% in order to match this goal and improve patient safety by resolving medication discrepancies. Prior to launching our study, our hospital AMRC rate was 67%. This project aimed to raise the AMRC rate to 90% by focusing quality improvement (QI) efforts on the Internal Medicine (IM) service, which cares for the majority of patients while having a historically low compliance rate (52%).
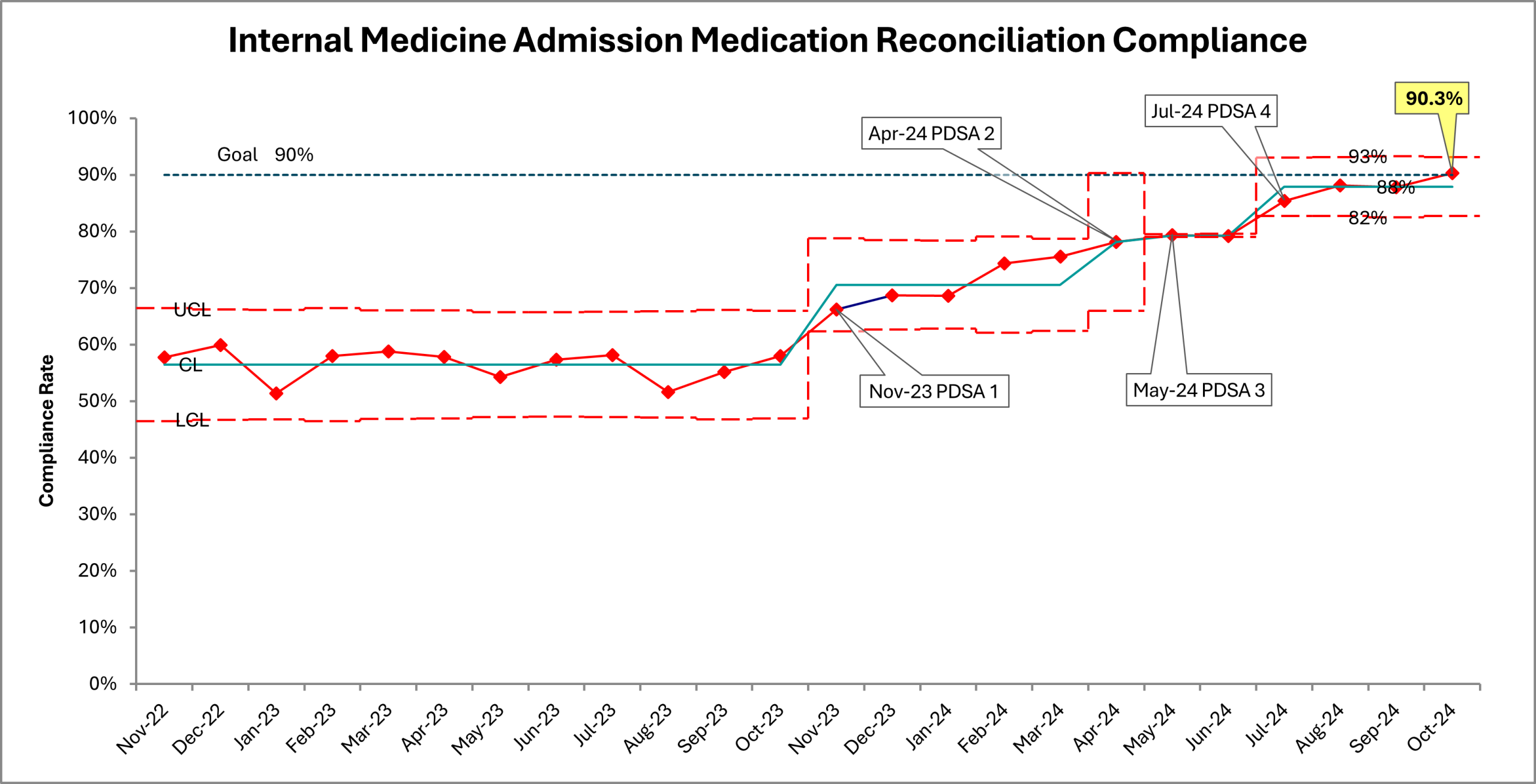
Methods: This QI study was conducted from Nov. 2023 to Oct. 2024 with a multidisciplinary team including a physician, pharmacist, nurse, and biostatistician. We implemented 4 Plan-Do-Study-Act (PDSA) cycles to raise AMRC across admissions to the IM service, which comprises 12 teams. The key element of our PDSA intervention was daily AMRC reporting, which identified patients’ medication history and reconciliation status. We created an innovative, robust reminder system tailored to remind IM teams of incomplete medication reconciliations. We analyzed changes in AMRC rates in Shewhart charts with process changes recorded at each new PDSA cycle and compared mean AMRC rates before and after implementation of QI interventions.
Results: The Shewhart chart (Figure 1) depicts monthly mean AMRC rates for IM service, the target of the QI intervention. Following the process change with PDSA 1 in Nov. 2023, the data indicate special cause variation with a sustained shift in IM team AMRC rates above the mean beginning in Feb. 2024 lasting through the end of the study period (over 9 consecutive data points). These patterns indicate a stable and predictable process with improved performance. Figure 2 depicts a comparison of IM team and hospital-wide means and ranges of AMRC rates before and after implementation of QI interventions. Prior to this study, the hospital-wide mean AMRC rate was 67% with a minimum compliance of 63%. The mean AMRC rate for IM alone was 56% with a minimum compliance of 52%. After implementation of team-specific daily compliance reports, IM service’s mean AMRC rate increased significantly to 79% (p<.0001), reaching a max AMRC of 90%. This propelled the hospital-wide mean AMRC rate upward to 82% (p<.0004) with a maximum of 91%, exceeding the goal set for the hospital by Oct. 2024.
Conclusions: Our hospital is one of the largest safety-net hospitals in the US, providing health care to a patient population comprised primarily of Medicaid, uninsured, migrant, and unhoused patients. Many have low health literacy, which encumbers our efforts to perform effective medication reconciliation. However, our study results show we were able to significantly increase IM service AMRC rate, which increased overall hospital AMRC rate through interdisciplinary collaboration and regular communication with IM teams with limited resources and staffing.