Background: Facilitating safe transitions of care is a common concern for the discharging hospitalist. Telephone calls are the most common method of contact for post-discharge outreach. These are labor-intensive and therefore limited in scope. To better support patients after hospital discharge, we designed and implemented a 30-day automated texting program. In a pilot study, this was associated with a significant reduction in acute care revisits.[1] We sought to test this program in a pragmatic randomized clinical trial.
Methods: A 2-arm, randomized clinical trial at 30 primary care practices in a single academic health system. Participants were established patients of the practices who were at least 18 years old, discharged from acute care hospitalization, and were considered by a health system risk score to be medium to high risk for adverse health events. Randomization was 1:1, balanced by practice. The control arm received usual care. Patients in the intervention arm received automated check-in text messages on a tapering schedule over a period of 30 days after discharge. If the automated messaging platform identified any patient needs, these were escalated to staff of the primary care practice to follow up. The main outcome was any acute care revisit, whether readmission or ED visit, within 30 days of discharge. Among patients randomized to the intervention arm, we additionally collected measures of engagement and satisfaction (via a 1-item Net Promoter Score (NPS) question, scored between -100 and +100).
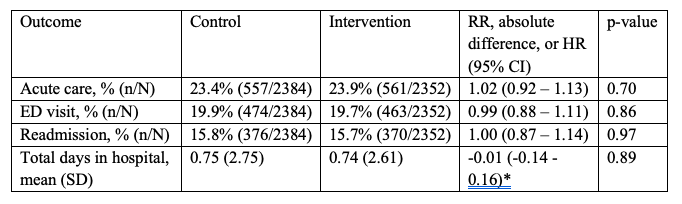
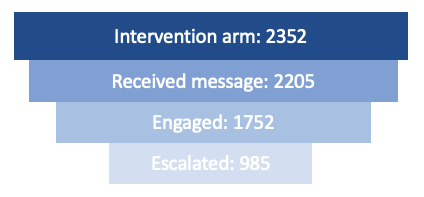
Results: There were 4736 participants: 2352 participants in the intervention arm and 2384 in the control arm. 2824 (59.6%) of the participants were female, 2322 (49.0%) were Black, and 2128 (44.9%) were white with a mean (SD) age of 65.4 (16.5). There was a mean (SD) length of index hospital stay of 5.5 (7.9). There were 557 (23.4%) 30-day acute care revisits in the control arm and 561 (23.9%) in the intervention group (RR 1.02, 95% CI 0.92 – 1.13). 79.5% of patients in the intervention arm answered at least one message and 41.9% had at least one need identified during the 30-day intervention period. There were 2130 patients who continued to the end of the 30-day intervention, of which 27.9% answered the NPS question for a score of +69.
Conclusions: There was no reduction in 30-day acute care revisits in this randomized clinical trial of a post-discharge automated texting program. However, patients were highly engaged and expressed strong satisfaction with the program. Future studies may examine the use of automated texting as a call replacement method through the lens of staff workload, since existing strategies for transitional care support are operationally burdensome,. In addition, given that a common concern for hospitalists coordinating discharge is the level of support in the home setting, their perspective on connected health strategies to provide more intensive support will be informative.