Background: The low published survival rate of pediatric in-hospital cardiopulmonary arrest (25-38%) 1 has led to the development of early warning systems (EWS) to identify patients at risk for deterioration. On our general pediatric unit, we implemented the published validated Children’s Hospital Early Warning System (CHEWS)2 in 04/2021. This composite scoring tool includes caregiver assessment and percentile ranges of vital sign abnormalities based on age-group2,3 and recommends a two-tiered alert system for scores >=3 (“yellow”) and >=5 (“red”). Within the first year of the initial rollout resident physicians and nurses reported alarm fatigue from the large number of calls related to CHEWS alerts, particularly due to asthma patients who had high scores but low disease severity. Alarm fatigue describes the desensitization of clinicians by overload of mostly false alarms and is a patient safety concern.4 Our QI project aimed to decrease the number of alerts by improving the specificity of CHEWS while preserving its benefits.
Methods: Our general pediatric unit comprises 30 beds with approximately 3500 admissions per year under the care of six different medical and surgical admitting services. In this retrospective cross-sectional study, electronic medical health record (EMHR) queries were used to quantitate patient subgroups 0-18yo with at least one elevated CHEWS score at “yellow” and “red” threshold as the primary metric as a correlate to alarm frequency. As a secondary metric, a query on pediatric patients treated on the acute asthma clinical pathway was used, and monthly rates of transfers to pediatric intensive care served as balancing metric.
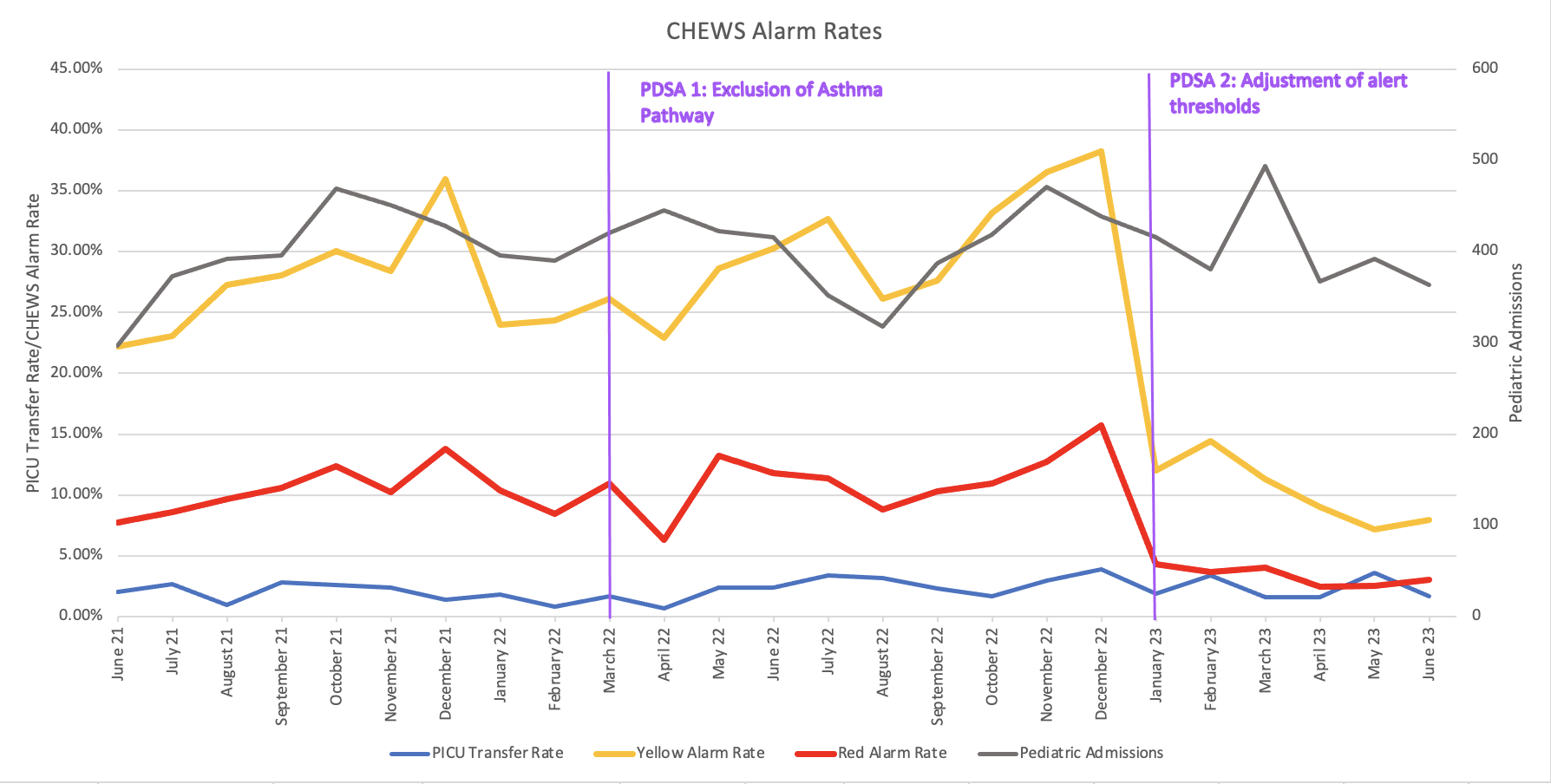
Results: Our first PDSA cycle focused on analysis of asthma patients: While rates of elevated CHEWS scores in the general pediatric inpatient population were 32% and 12% for “yellow” and “red” alerts, patients on the asthma pathway had significantly elevated rates of 83% and 58% respectively. Despite elevated CHEWS scores, asthma pathway patients rarely need escalation of care and have an average LOS < 2d. The elevated scores can be explained by the iatrogenic positive chronotropic effect of bronchodilators. Also, a disease-specific asthma score is used in the pathway. Hence, in 03/2022 our first intervention was to exclude asthma pathway patients from CHEWS scoring. As pediatric inpatient admission volumes returned to normal post COVID-19 the proportion of elevated CHEWS continued to rise. In winter 2022/23, up to 40% (16%) of patients admitted to the pediatric floor reached scores of >=3 (>=5) causing significant alert fatigue (Fig. 1). In 01/2023, our second intervention increased the thresholds for “yellow” and “red” alerts by one point respectively. This adjustment decreased the average alarm rate to 11% for “yellow” and 3% for “red scores”. The rate of transfers to higher level of care and code events did not change throughout the two PDSA cycles.
Conclusions: By applying PDSA methodology, we were successful in safely decreasing the rate of CHEWS alerts from pre-intervention 30% to post-intervention 11% through elimination of asthma exacerbation patients and adjusting threshold scores for “yellow” and “red” alerts based on local data. The limitations of our analysis are that the number of elevated alarms were potentially underestimated by the available reports and that no primary data on alarm fatigue was collected.