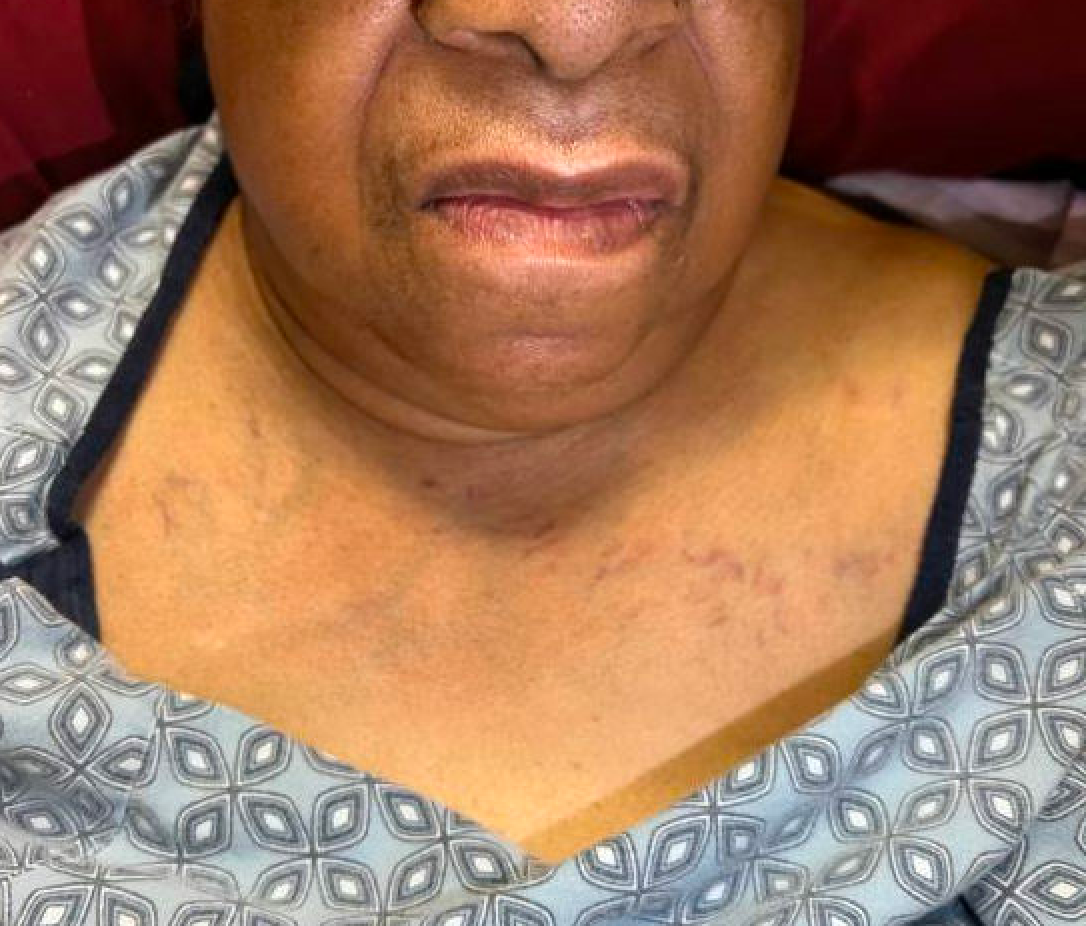
Case Presentation: An 82 y/o woman with Grave’s disease (diagnosed 3 years prior), h/o thyrotoxicosis, CKD stage 4, HTN, DM2, PAD s/p right AKA, HFpEF, and dementia presented to the ED with worsening bilateral upper extremity edema and new-onset right facial swelling. She denied dyspnea, dysphagia or voice change. Her arm edema was previously managed with diuretics. Two months prior, she was diagnosed with a right IJ thrombus and started on apixaban. RUE US revealed an unchanged right IJ thrombus. CXR showed enlarged cardiac and mediastinal contours with leftward deviation and narrowing of upper thoracic trachea and new mild pulmonary edema. CT SVC protocol revealed severe narrowing at the bilateral brachiocephalic veins at their junction with the subclavian and IJ veins with collateral flow in the anterior chest wall. A multilobular goiter extended into the superior mediastinum with mild mass effect on the trachea. The patient had bilateral brachiocephalic vein compression on account of her enlarging multinodular goiter with subsequent mimicking of superior vena cava (SVC) syndrome. She was a poor candidate for thyroidectomy. Thyroid artery embolization was not recommended given prolonged time to yield response. Placement of bilateral stents to BC veins was offered as a temporizing measure but declined by the patient due to improvement with conservative measures. She was discharged with endocrinology follow-up for consideration of radioactive ablation, and ongoing goals of care discussions.
Discussion: A substernal goiter is enlargement of the thyroid gland that extends into the mediastinal cavity, past the sternal notch (1,2). The incidence of substernal goiters among patients with goiters is approximately 2-19%. They are typically seen in the 5th-7th decades of life and have a 4:1 female predominance (3,4). Many patients are asymptomatic and incidentally diagnosed from imaging (5). These masses are typically slow growing, but over time can compress adjacent structures, including the trachea, esophagus and venous structures leading to dyspnea, dysphagia, dysphonia (compression of the recurrent or superior laryngeal nerve), SVC syndrome, and thrombus formation (6). Per the American Thyroid Association, definitive treatment is complete surgical thyroidectomy. Indications for surgery include current compressive symptoms, complications from progressive enlargement, or suspicion for malignancy (2). The most common complications of thyroidectomy include hypocalcemia, laryngeal nerve injury and post-operative bleeding. The patient was not a surgical candidate due to her significant cardiopulmonary comorbidities. Due to the extent of her goiter, a midline sternotomy would be required for complete excision, rather than a cervical approach, which also carries higher risk of complications. Other potential treatment options include radioactive iodine (RAI) and antithyroid drugs, the latter of which would be ineffective with this patient. An alternative treatment option involves thyroid artery embolectomy which has been shown to reduce thyroid volume and size by 50% in 6 months (7).
Conclusions: SVC-like symptoms in a patient with a substernal multinodular goiter is a rare diagnosis. Close monitoring and surveillance in patients with known multinodular goiters could even further reduce the incidence. When diagnosed, prompt surgical treatment is the recommended treatment as recurrence approximates 0%.