Background: Successful discharge practices and avoidance of readmission requires attention to social needs and care coordination with outpatient care providers. While national programs have attempted to identify interventions within the care continuum to prevent readmission, these programs rarely involve inpatient hospitalists. While robust requirements for certain care transitions processes such as medication reconciliation and discharge summaries are emphasized by regulating bodies, few guidelines exist regarding optimal discharge communication practices between hospitalists and primary care physicians (PCP’s). Challenging the notion of “follow up with PCP”, as the reflexive discharge practice, our hospitalist group studied the patterns of current discharge practices and ways to enhance our hospitalists’ skill sets.
Purpose: Our goal is to standardize hospitalist discharge practices to improve post discharge care coordination, increase attendance at follow-up appointments, and decrease hospital utilization and readmissions.
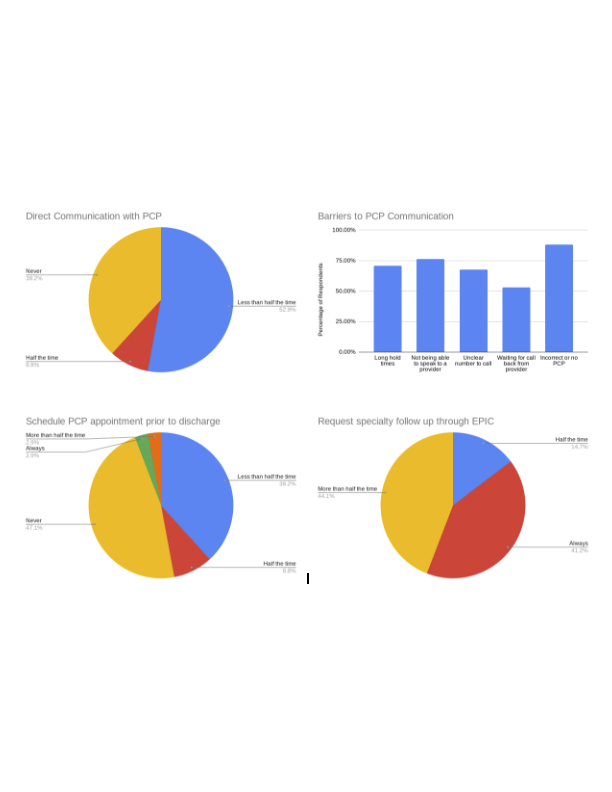
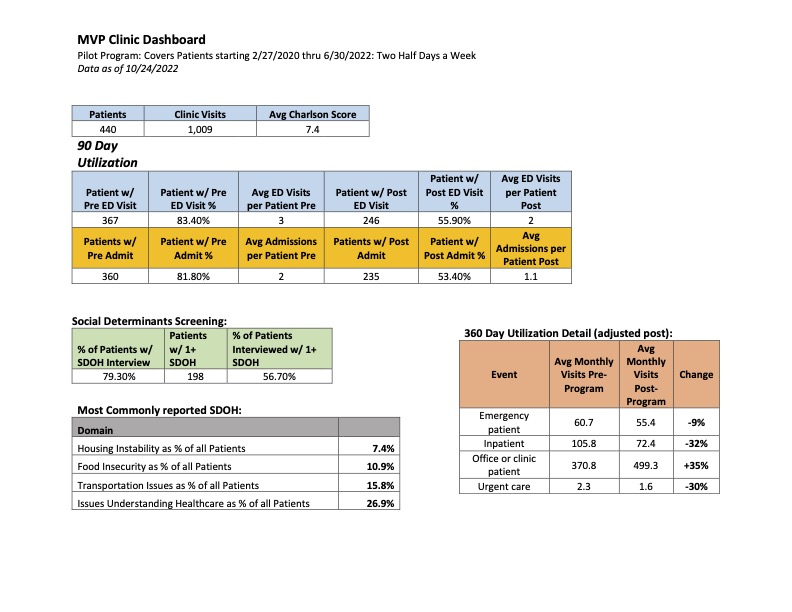
Description: Our group of 61 hospitalists practice in a large, urban, safety-net academic medical center. Readmissions rates are 12 – 15% within 30 days, with higher rates for heart failure patients (over 20%). To study current practices, the group was surveyed. Responses reveal that more than 50% of respondents (n=41) do not regularly communicate with PCP, and 47% report never scheduling a PCP appointment prior to discharge. Institutional reports from our practice plan noted high numbers of subspecialty appointment requests at the time of discharge (3.2 appointments per patient), with < 20% of requests resulting in completed visits. Qualitative review of barriers to care planning and communication included: unclear follow up plans, long phone wait times with PCP offices, and lack of patient knowledge or access to a PCP. Based on survey responses, we are creating a tool, in partnership with population health, to identify correct PCPs and PCP’s preferred communication methods. In parallel, we created a readmissions reduction clinic for patients with frequent hospital visits. Social drivers of utilization such as food insecurity, housing instability, and lack of access to transportation significantly impact inpatient utilization. The readmission reduction (MVP) clinic is staffed by a hospitalist and is supported by a network of community health workers (CHW). Physicians perform transition of care visits which include social determinants of health (SDOH) screening and response, assessment of medication access and adherence, intensive disease management and education, and warm handoff to long term PCP care. The hospitalist coordinates with CHW team to address any SDOH needs. For patients who enter the program, a 32% reduction of inpatient utilization has been observed and sustained. Details of our MVP clinic outcomes and survey results are attached.
Conclusions: Shifting culture to prioritize post-discharge care planning and coordination is essential to a successful hospital discharge. Alignment with health system goals of reducing readmissions, standardizing PCP communication practices, developing faculty care transitions skills, and including hospitalists in post discharge programs are essential for hospitalist practice. Based on our MVP clinic pilot program, we believe increased patient engagement via referrals to the program, increased care planning discussions with PCPs and patients, and increased attention to SDOH needs can improve patient outcomes.