Background: Patients with undifferentiated but stable clinical presentations may manifest sepsis “time zero” (T-0) or the onset of sepsis-defining conditions while undergoing further evaluation in observation units (OUs). Since these units are often designed to facilitate diagnostic and clinical risk assessments, we hypothesize that patients experiencing T-0 while in OUs will likely experience similar or better quality of care and outcomes compared to patients experiencing T-0 while admitted to general inpatient units (GIUs).
Methods: We retrospectively identified patients admitted to a large academic hospital between July 2021 and October 2023 with sepsis based on the Centers for Disease Control and Prevention (CDC) surveillance criteria. We collected demographic and clinical data on those with community acquired sepsis, defined as experiencing Centers for Medicare and Medicaid Services (CMS) T-0 within the first 48 hours of hospitalization. We excluded patients who experienced T-0 while in the emergency department. We compared characteristics and CMS Severe Sepsis and Septic Shock Management Bundle (SEP-1) 3-hour compliance of patients experiencing T-0 while in OU vs GIU using Pearson chi-squared test, Wilcoxon rank sum test, and Fisher’s exact test. We also fitted a logistic regression model for SEP-1 compliance to assess association with OU vs GIU at T-0 while adjusting for age, sex, Charlson comorbidity score, and presence of septic shock. Primary outcomes were in-hospital and 30-day mortality. We assessed associations between these primary outcomes and T-0 in OU using multivariate logistic regression while adjusting for age, sex, Charlson comorbidity score, presence of septic shock, and SEP-1 3-hour bundle compliance.
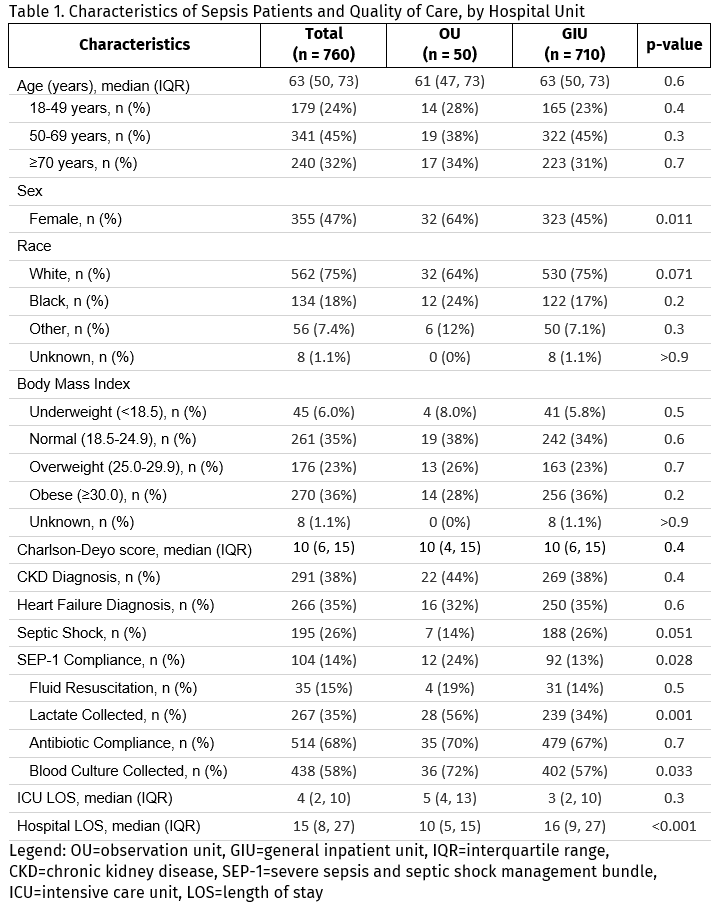
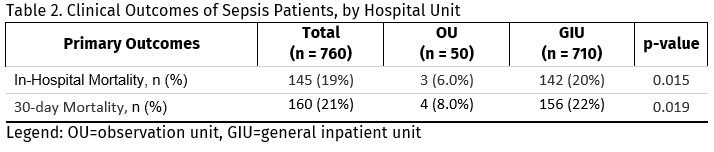
Results: Of 760 patients with community acquired sepsis, 7% (50) experienced T-0 while in OU and 93% (710) in GIU. Patients in both groups had similar distribution in age, race, and body mass index (Table 1). Those in OU had similar comorbidity score compared to those in GIU (median, 10 vs. 10, p=0.4). Hospital length of stay was shorter for patients experiencing T-0 in OU vs. GIU (median, 10 days vs. 16 days, p< 0.001). SEP-1 bundle compliance was higher among patients experiencing T-0 in OU compared to those experiencing T-0 in GIU (24% vs. 13%, p=0.03). After accounting for age, sex, comorbidity score, and presence of septic shock, the odds of SEP-1 compliance were higher in OU compared to GIU (adjusted odds ratio [aOR], 2.27; 95% confidence interval [CI], 1.09 – 4.44). There were fewer deaths during hospitalization and within 30-days among patients that manifested sepsis in OU compared to those in GIU (Table 2). Adjusted for a priori selected covariates, patients experiencing T-0 while in OU had lower odds of in-hospital mortality (aOR, 0.29; 95% CI, 0.07 - 0.90; p=0.056) and lower odds of 30-day mortality (aOR, 0.33; 95%CI, 0.09 - 0.88; p=0.047).
Conclusions: In this single site study, patients with community acquired sepsis who experience T-0 while in an observation unit more frequently receive SEP-1 compliant care and have lower odds of 30-day mortality compared to those experiencing T-0 in general inpatient units. While there is opportunity to improve SEP-1 compliance in both OU and GIU, the variation in performance between both settings appears to be related to differences in unit characteristics. Further studies are needed to identify specific unit structural and operational features associated with increased sepsis recognition and early treatment.