Background: Hospital readmissions are a significant healthcare concern, particularly for patients harboring liver cirrhosis. Optimizing discharge planning and transitional care management for this population requires a detailed understanding of the factors associated with readmission risk, stratified by disease severity. Elixhauser Comorbidity Index v2024.1 guided identification of patients with standardize mild versus moderate-severe cirrhosis plus respective comorbidity burden. Primary hypothesis was that readily available EMR features (demographics, laboratory results within 24h, and administrative data) could be identified and modeled to predict 30-day readmission risk in hospitalized patients with mild versus moderate-severe cirrhosis. Secondary hypothesis was predictive strength of these features differed across severity.
Methods: Data to address hypothesis were extracted from EMR under IRB exemption. Generalized regression with LASSO and response surface methodology identified from putative and biologically plausible features those associated (p<.05) with 30d readmission in patients harboring mild versus moderate to severe cirrhosis. Univariate regression modeling generated Youden Index to identify cut point with optimal sensitivity and specificity for each associated feature. Boosted Tree ensemble modeling estimated each feature’s proportion (%) of variance explained (VE) in overall model’s accuracy (R2) to estimate risk for 30d readmission stratified by cirrhosis severity. Continuous data summarized with median [IQR] were compared using Kruskal–Wallis test. Discrete data summarized as proportions were compared with chi-square test. Statistical significance was considered at p< 0.05 with confounders controlled including concurrent COVID-19.
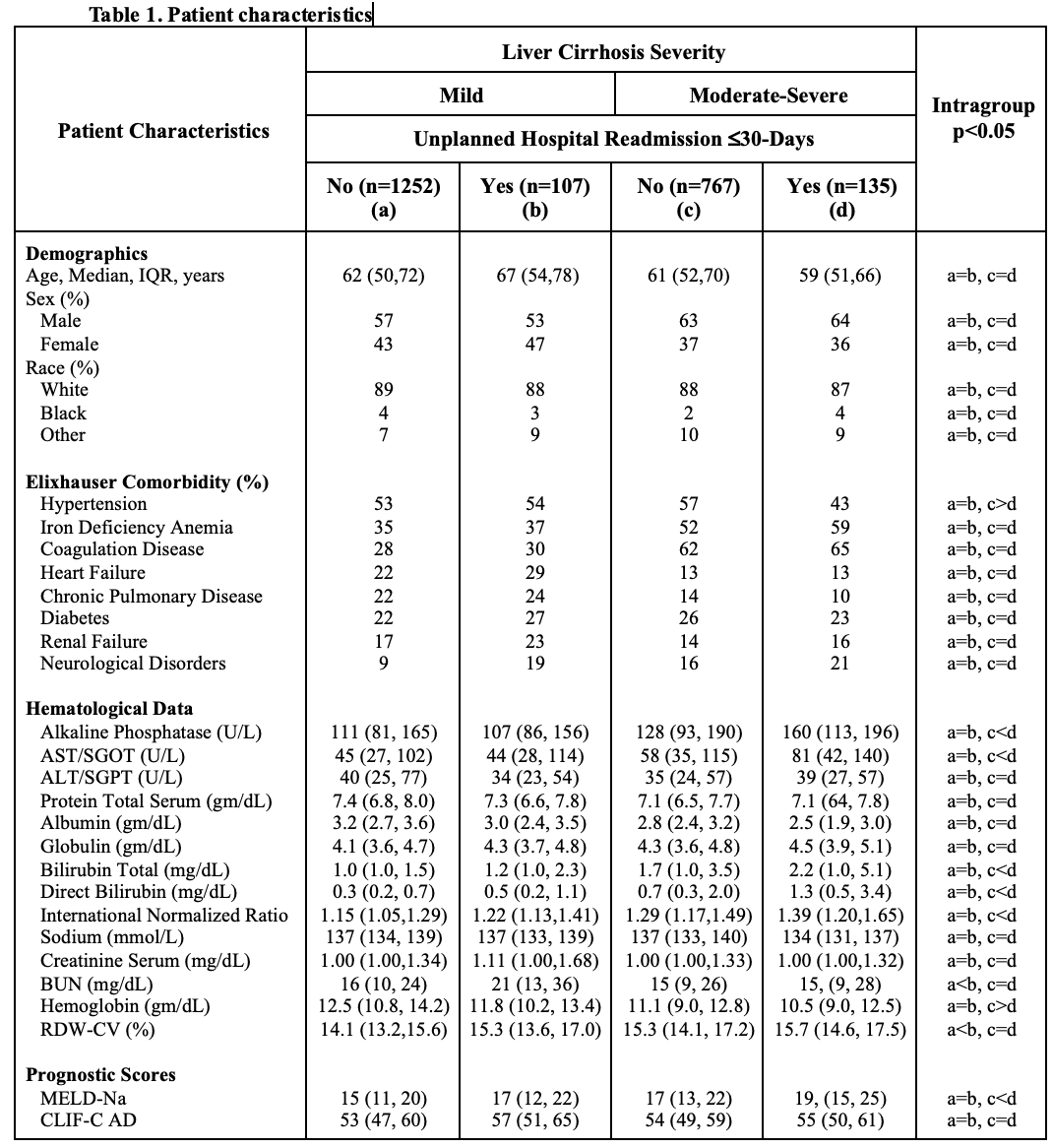
Results: Among 2,261 liver cirrhosis patients, 1,359 (60%) versus 902 (40%) respectively expressed mild versus moderate-severe disease exhibiting 30d readmission rates of 7.9% versus 15.0%. Patient characteristics across disease severity are presented in Table 1. Boosted Tree modeling accuracy (R2) along with feature cut points and variance explained (VE%) indexed to cirrhosis severity are provided in Table 2.
Conclusions: The study identified readily available EMR features with varying predictive power for 30-day readmission in patients with cirrhosis, stratified by disease severity. Specifically, comorbidity burden (Elixhauser Comorbidity Index) was a dominant predictor in the mild cirrhosis cohort, while anemia (hemoglobin levels) was a dominant predictor in the moderate-severe cirrhosis cohort. Other notable predictors include markers of kidney dysfunction (BUN/Albumin Ratio), liver disease severity (MELD-Na Score), and nutritional status (Albumin/Globulin Ratio). Elevated AST/ALT ratios may indicate specific etiologies requiring targeted interventions. Prolonged hospitalizations (Hospital LOS/MS-DRG GMLOS Ratio) and high CLIF-C AD scores warrant closer monitoring and proactive management to mitigate readmission risk. Early identification of these risk factors, particularly when a patient’s progress deviates significantly from the Medicare Severity Diagnosis Related Group Geometric Mean Length of Stay, can siren complications or need for more intensive interventions. Both models exhibit moderate prediction ability suggesting that while these factors are important, other unmeasured variables also contribute to readmission risk.