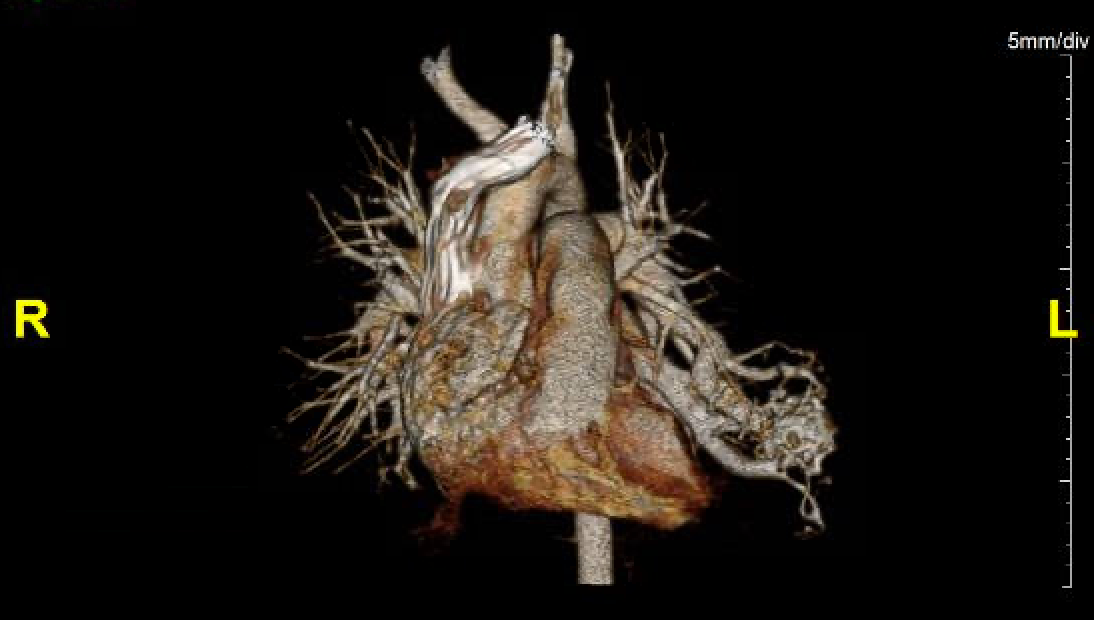
Case Presentation: A 3-year-old male with past medical history of mild persistent asthma and allergic rhinitis presented with persistent hypoxia. He had a history of multiple prior hospitalizations for hypoxia, mainly in the setting of acute respiratory illness. At an outpatient cardiology visit, he was found to be hypoxic to 87%, though echocardiography was unrevealing for any intracardiac lesion or interatrial shunt. Pertinent family history included the patient’s mother, three maternal siblings, and maternal grandmother had clinical diagnoses of hereditary hemorrhagic telangiectasia (HHT, Osler-Weber-Rendu syndrome).On admission, the patient was hypoxic with mild subcostal retractions and improved on oxygen via nasal cannula. CBC was notable for elevated hemoglobin of 14.4. Physical exam findings were notable for clubbing of the fingers bilaterally, most prominently in the thumbs. Chest X-ray showed mild peribronchial thickening consistent with acute viral illness.Given the patient’s strong maternal family history of HHT, further workup was performed to evaluate for the presence of arteriovenous malformations (AVMs) as a contributing factor to his hypoxia. Chest CT angiography revealed a large vascular lesion in the left lower lung lobe extending from the left pulmonary artery with evidence of contrast shunting, consistent with a high flow lesion or AVM. A cardiac catheterization procedure was performed with device occlusion of two feeder vessels to the high-flow pulmonary lesion. Post-procedure, the patient experienced immediate, marked clinical improvement, with SpO2 rising to 98% on room air. His supplemental oxygen requirement was eliminated, and his mother noted increased energy and decreased shortness of breath with activity. The patient was diagnosed with chronic hypoxia due to a large pulmonary AVM in the setting of suspected HHT. Subsequent genetic follow-up identified that the patient had the same variant of unknown significance as his maternal grandmother, which may relate to their familial HHT.
Discussion: HHT is a rare, autosomal dominant disorder characterized most commonly by mucocutaneous telangiectasias and visceral AVMs with a prevalence of 1 in 5000 to 8000. The diagnosis can often be made clinically in adults via the 2000 Curaçao criteria by international consensus. The disorder has high penetrance by middle adulthood, but variable penetrance and presentation in childhood. The 2020 Second International HHT Guidelines recommend that pediatric patients who have HHT or have parents with HHT be screened regularly for pulmonary and brain AVMs and treated as needed with embolization.This patient did not demonstrate the classic findings of frequent epistaxis or mucocutaneous telangiectasias on his fingers, lips, or oral cavity. Instead, he presented with signs of chronic hypoxia (elevated hemoglobin, digital clubbing, decreased energy) and recurrent acute episodes of hypoxia, exacerbated during respiratory illness. His hypoxia can be attributed to his large pulmonary AVM, likely a sequela of HHT, as he experienced immediate symptom relief with vessel occlusion.
Conclusions: It is important for pediatricians to keep HHT on the differential for pediatric patients with symptoms of chronic hypoxia, especially those with strong family history. Screening should be performed for brain and pulmonary AVMs for all pediatric patients who may be at higher risk for HHT based on family history and associated symptoms, regardless of the presence of visible superficial telangiectasias.