Background: The 2014 ACC/AHA Perioperative Guidelines suggest using the Revised Cardiac Risk Index (RCRI), myocardial infarction or cardiac arrest (MICA), or American College of Surgeons (ACS)-NSQIP calculators for combined patient-surgical risk assessment. However, there is no published data comparing their performance.
Methods: We retrospectively reviewed records of 663 patients seen in our preop clinic who underwent various intermediate-high risk noncardiac surgeries. We calculated scores for the risk indices/calculators and recorded in-hospital and 30-day cardiac complications (MI, cardiac arrest, pulmonary edema). These scores were then compared based on predicted and observed complications.
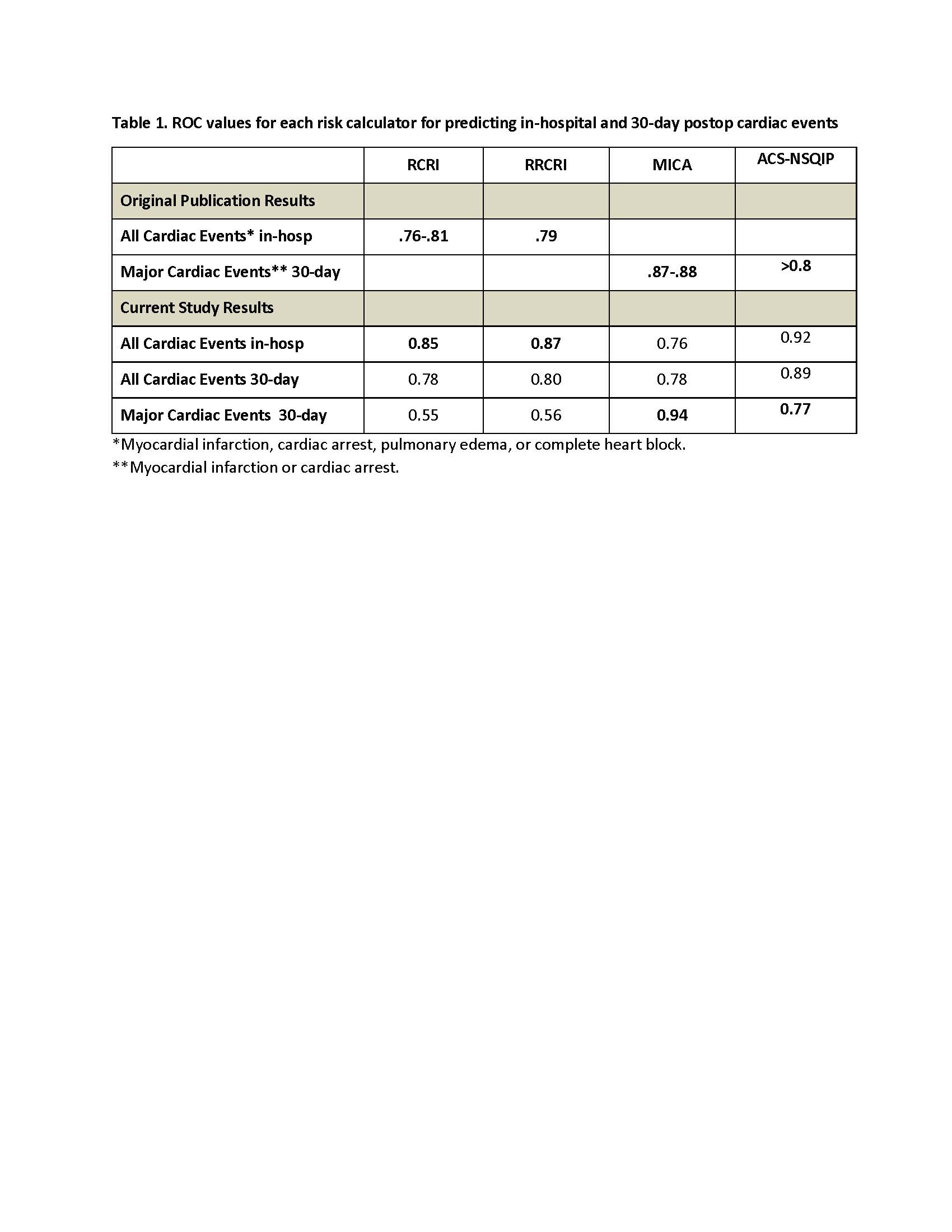
Results: 14/663 (2.1%) of patients developed cardiac complications of which 11 occurred during hospitalization. As per ACC guidelines, low risk was defined as complication rates of <1% and elevated risk was >1%.The calculators classified 93-98% of patients as low risk with corresponding complication rates of 0.6-1.2%, and 2-7% patients were classified as elevated risk with complication rates of 2.1-23.1%. For predicting complications as defined in the original publications, ROC curves for RCRI and Reconstructed RCRI were 0.85 and 0.87 for in-hospital complications, and the ROC values were 0.94 and 0.77 for MI/cardiac arrest within 30 days for MICA and ACS-NSQIP. The ROCs for all risk calculators in our study were similar to values in the original studies (Table 1). For patients with a LOS<2 days or undergoing low risk procedures, the RCRIs were non-discriminative whereas the performance of other calculators was similar to the overall cohort. The number of patients classified as elevated risk (>1%) as per ACC Guidelines was lower for MICA than for other scores, but incidence of cardiac events in these patients was higher for MICA.
Conclusions: All four risk calculators performed well but tended to underestimate cardiac events in elevated risk patients, although most patients did well after surgery. Our results demonstrate that the RCRIs predict what they were designed to do – predict in-hospital MI, VF/CA, pulmonary edema, and CHB in patients undergoing major noncardiac surgery with an expected LOS>2 days. However, when used inappropriately for lower risk procedures with LOS<2 days, they overestimate risk and could potentially lead to unnecessary cardiac tests. THE MICA may be the most reliable in selecting higher-risk patients according to ACC Guidelines. However, any of these scores can help define low risk patients in whom further cardiac testing is unnecessary. One limitation of our study was the low incidence of cardiac complications, and future studies should evaluate a larger database to better define any differences between these risk calculators.