Background: Adverse events (AE) are common during care transitions (19-28%) in patients with multiple chronic conditions (MCC) and often lead to unanticipated healthcare resource utilization after discharge. While early indicators of these AEs include new and worsening symptoms, systematic monitoring of patient-reported symptoms is lacking. The 21st Century Cures Act mandates the healthcare industry to adopt standardized data definitions and modern application programming interfaces (APIs), offering the potential to engage patients in their care in part by accessing their health data. In theory, interoperable digital health apps that use APIs have the potential to individualize assessment of risk for AEs during transitions by combining electronic health record (EHR) data with responses from validated patient-reported outcome (PRO) questionnaires. Escalating these potentially high-risk states to care team members involved in the transition may lead to earlier intervention.
Purpose: As part of our AHRQ project (R01-HS028662), we proposed developing a prediction model of post-discharge AE to be used in a digital health app derived primarily from EHR data elements and the 10-item Global Health PRO questionnaire. Additionally, the collection of PRO data and reported symptoms presents an opportunity to proactively monitor patients during the post-discharge period. We describe our process for designing a prediction algorithm to escalate potential AEs during transitions.
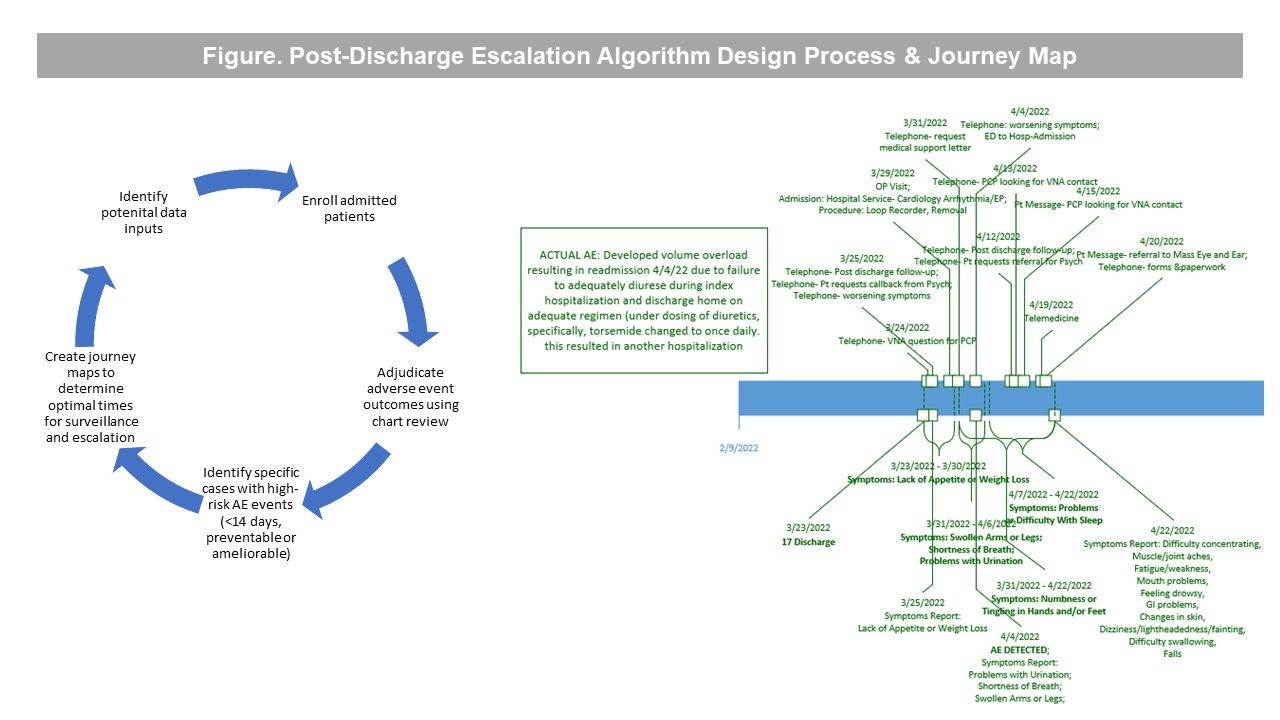
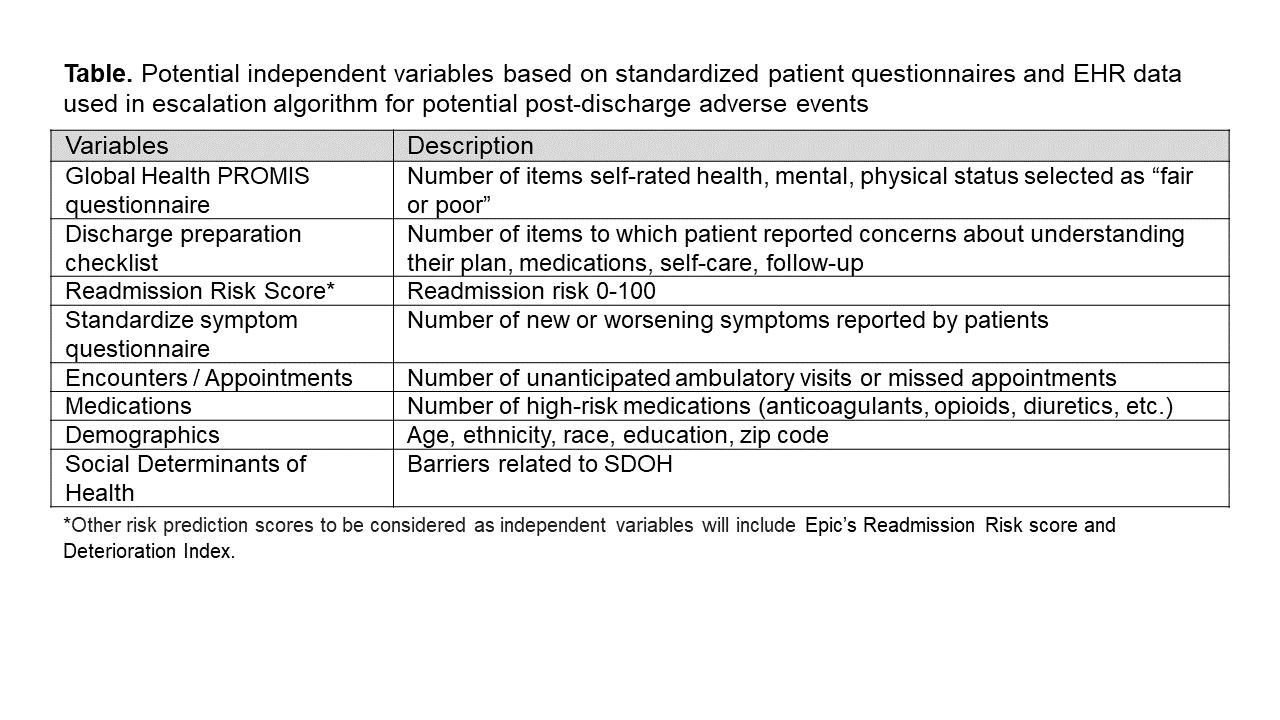
Description: Our design process involves 5 steps (Figure). First, we enroll hospitalized patients, have them complete the Global Health PRO questionnaire, and follow their course for 30-days after discharge. We use a validated chart review process to identify AEs during the 30-days after discharge. Of 101 cases adjudicated to date, 8 (7.9%) had at least one preventable or ameliorable AE within 14-days of discharge which was associated with unanticipated utilization events (i.e., ED visit, readmission). From analysis of 10-item Global Health PRO responses in these 8 patients, 2 (25%) reported that their overall health was “Fair” or “Poor”, and their mean T-scores (0-100) for mental and physical health were 45.7 and 41.8, respectively. The average number of symptoms reported within 14-days was 3.6 per patient (mostly commonly shortness of breath and swollen legs). Our clinical engineer used journey mapping (Figure) to analyze timing of reported symptoms and utilization events to understand when to administer questionnaires to collect data and other types of EHR data (Table) that could be used to inform our escalation algorithm.
Conclusions: The use of electronic PROs for post-discharge symptom monitoring, AE surveillance, and escalation is novel and potentially transformative–it will empower patients to clearly understand and trend their individual risk of AEs, provide tailored self-care guidance, and help them determine when to seek help after discharge. Our next steps are to confirm data inputs / variables with our stakeholders, ensuring that they correspond to USCDI road map to maximize interoperability.