Background: Pain is assessed by nurses through either reported or observed intensity. Self-reported assessments, specifically a numeric score, are the gold standard and preferred to behavioral assessments. Disparities in the assessment and management of pain across race, ethnicity, and language status are prevalent, but we do not know how actual numeric pain scores vary and how they relate to administered opioid pain medication.
Methods: This was a retrospective cohort study of all adults discharged from the acute care inpatient general medicine service from January 2013-September 2021 at an 800-bed urban teaching hospital. Nurses can select one of several pain assessment tools to document patient’s pain. The most common is the Numeric Rating Scale (NRS), a 0-10 scale, where a patient reports their pain intensity. We collected all documented pain assessment and covariate data including patient demographics, medical, and hospitalization related variables. Our primary predictors were self-reported race/ethnicity (white, Black, Asian, Latino, Native Hawaiian/Other Pacific Islander, American Indian/Alaska Native, Multiracial, Other/Unknown) and whether the patient had limited English proficiency (LEP). We reported three outcomes. First, we used logistic regression to examine the odds of receiving a “0” pain score compared to a score ≥1. Second, we used negative binomial regression to predict the mean numeric pain score. Third, we used negative binomial regression to predict the average morphine milligram equivalents (MME)/day. All models included multivariable regressions, controlling for demographic (age, gender, race/ethnicity, LEP status, and insurance), medical, and hospitalization related covariates (year of study, primary team, diagnoses of cancer pain or substance use disorder, prior opioid or medication for opioid use disorder use, end of life care, ICU transfer, pain or palliative care consult, and Elixhauser comorbidity index.)
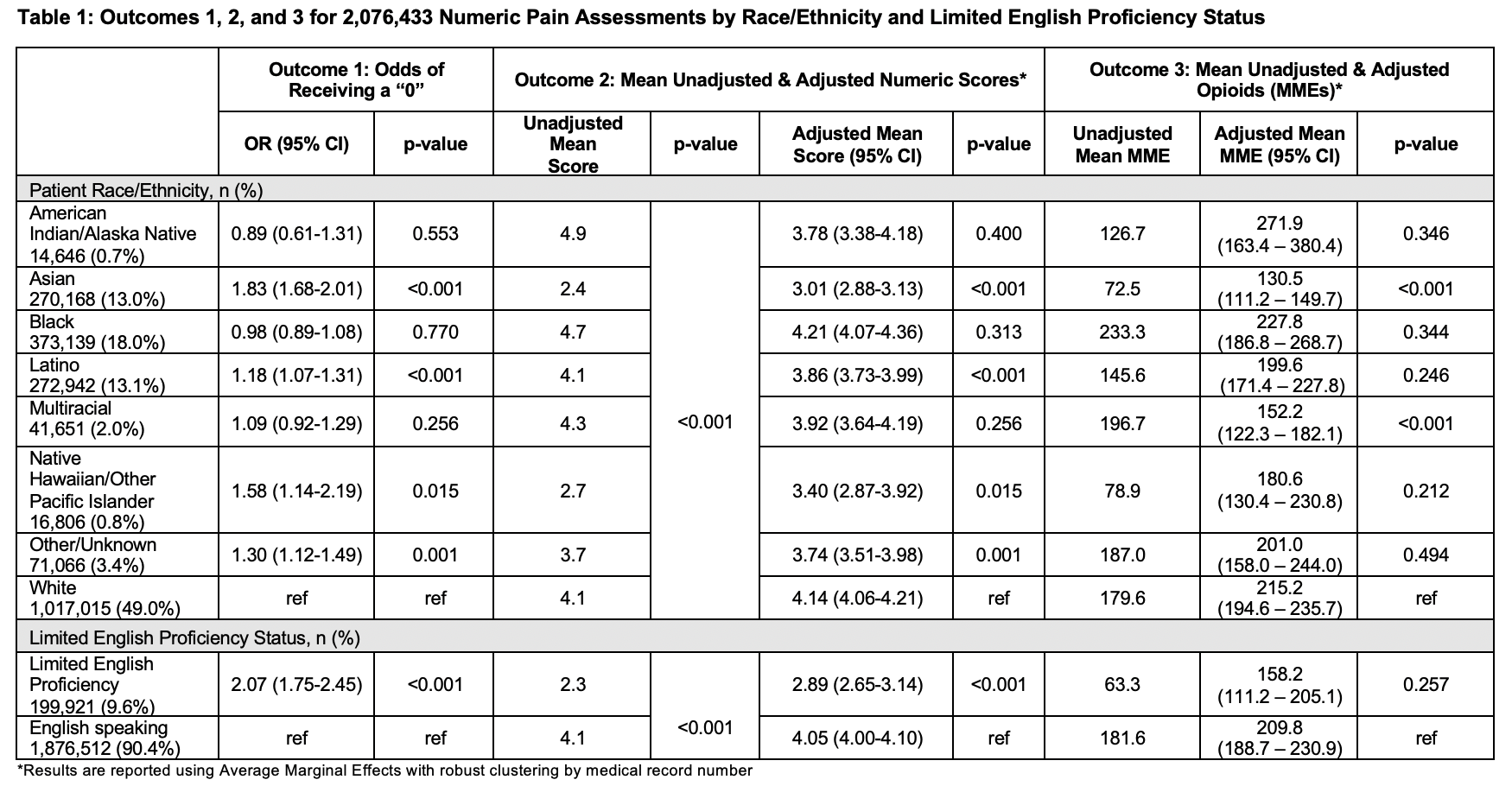
Results: We identified 61,576 patient hospitalizations with a total of 3,639,811 pain assessments. NRS assessments were most common at 2,076,433, comprising 57.0% of all assessments. For outcome 1, we found significant differences with Asian (OR 1.83, 95% CI 1.68-2.01) and LEP patients (OR 2.07, 95% CI 1.75-2.45) more likely to report a 0. Latino, Native Hawaiian/Other Pacific Islander, and patients identified as Other or Unknown were also more likely to report a 0. For outcome 2, Asian (3.01, 95% CI 2.88-3.13), Latino (3.86, 95% CI 3.73-3.99), Native Hawaiian/Other Pacific Islander (3.40, 95% CI 2.87-3.92), and patients identified as Other/Unknown (3.74, 95% CI 3.51-3.98) had lower adjusted mean pain scores compared to white patients (4.14, 95% CI 4.06-4.21). LEP patients (2.89, 95% CI 2.65-3.14) had a lower adjusted mean pain score than English speaking patients (4.05, 95% CI 4.00-4.10). For outcome 3, Asian (131 MME, 95% CI 111-150) and Multiracial (152 MME, 95% CI 122-182) patients received fewer adjusted mean daily MMEs than white patients (215MME, 95% CI 195-236). There were no significant differences in MMEs for LEP vs English speaking patients. (Table 1)
Conclusions: Asian patients and patients with LEP were more likely to have a pain score of “0” and had lower mean numeric scores documented by nursing staff while hospitalized. Asian patients also received fewer opioids, accounting for reported pain scores and other covariates, demonstrating disparities in opioid prescribing.