Background: People experiencing homelessness (PEH) face barriers to accessing regular ambulatory care, which increases their risk of having poorly controlled chronic medical conditions and contributes to high acute care utilization. The role of field-based homeless healthcare teams in improving hypertension and diabetes control and reducing acute care utilization (e.g., emergency department [ED] visits, inpatient hospitalizations) is not well-described. The objectives of this study are to determine if encounters with a Los Angeles-based field-based homeless healthcare team are associated with improved hypertension and diabetes control and to determine if encounters with the team are associated with reduced ED and inpatient encounters.
Methods: We performed a cross-sectional analysis of adult patients aged 18 years or older treated between January 2022 and April 2024 by the Homeless Healthcare Collaborative (HHC), UCLA Health’s field-based homeless healthcare team. Data for this study were based on electronic health records (EHR). We examined patients with a diagnosis of hypertension (based on ICD diagnosis in EHR or having at least two blood pressure readings >= 140/90) or diabetes (based on ICD diagnosis in EHR, HgbA1c >6.5% or prescription for an antiglycemic medication), a minimum of 3 encounters with HHC and a minimum of 2 blood pressure or HgbA1c readings. We performed pre-post analyses comparing blood pressure and HgbA1c readings between the first and last encounters with HHC. In a separate analysis, we examined patients with at least one emergency department (ED) or inpatient encounter at UCLA Health prior to their first HHC encounter. We compared the number of ED encounters per patient 6 months before and after their first HHC encounter, stratified by the number of ED encounters prior to their first HHC encounter. We also compared the number of inpatient encounters per patient 12 months before and after their first HHC encounter, stratified by the number of inpatient encounters prior to their first HHC encounter. Comparisons were tested using paired t-tests and Wilcoxon rank-sum testing.
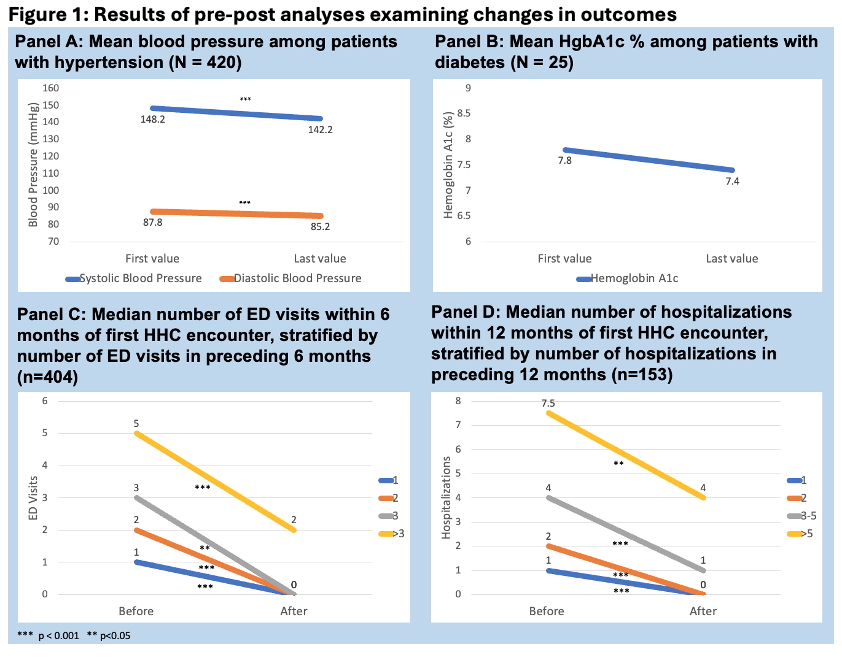
Results: Overall, HHC treated 5192 patients between January 2022 and April 2024 (Table 1). Among the hypertension group (n=420), mean systolic and diastolic blood pressure significantly decreased by 6 and 2.6 mmHg, respectively, between first and last encounter with HHC (p< 0.001 for both) (Figure 1). Among the diabetes group (n=25), HgbA1c% decreased from 7.8% to 7.4%, though this difference was not statistically significant (p=0.26). Median ED encounters 6 months after the initial HHC encounter significantly decreased compared to the median ED encounters 6 months prior to the HHC encounter across all strata (patient n=404) (Figure 1). Median inpatient encounters 12 months after the initial HHC encounter also significantly decreased compared to median inpatient encounters prior to the initial HHC encounter across all strata (patient n=153) (Figure 1).
Conclusions: Field-based homeless healthcare has the potential to improve blood pressure and diabetes control for PEH who might otherwise not have access to ambulatory care. Field-based homeless healthcare may also contribute to reducing acute care utilization among PEH. Further research is needed to analyze outcomes across multiple field-based homeless healthcare teams and compare outcomes between PEH who encounter field-based homeless healthcare and those who do not receive services from these teams.