Background: “Geographic rounding” describes physicians focusing on patient care in a single hospital unit. Studies have suggested that geographic rounding may improve efficiency and communication. Prior to our pilot, physicians at EUHM were seeing patients distributed across 13 units making rounding inefficient and care coordination challenging.
Methods: We designed a geographic-based rounding system on unit 72, a permanent 19-bed med/surg unit at EUHM. The patient population includes primarily neurologic and psychiatric diagnoses, with other med/surg overflow to ensure capacity is met. All patients on the unit were assigned to one hospital medicine team/attending with exclusion of the observation and teaching teams.A daily inter-disciplinary huddle was implemented involving social work, case management, nursing, and physicians with the goal of improving communication and identifying discharge barriers. We looked at 2 metrics: monthly average discharges and length of stay(time in bed). Baseline data covers 10/2022-8/2023 prior to huddle initiation (9-10/2023 unavailable due to epic transition). Current state includes 11/2023-5/2024. Outliers of >31 days were removed from time in bed data sets.
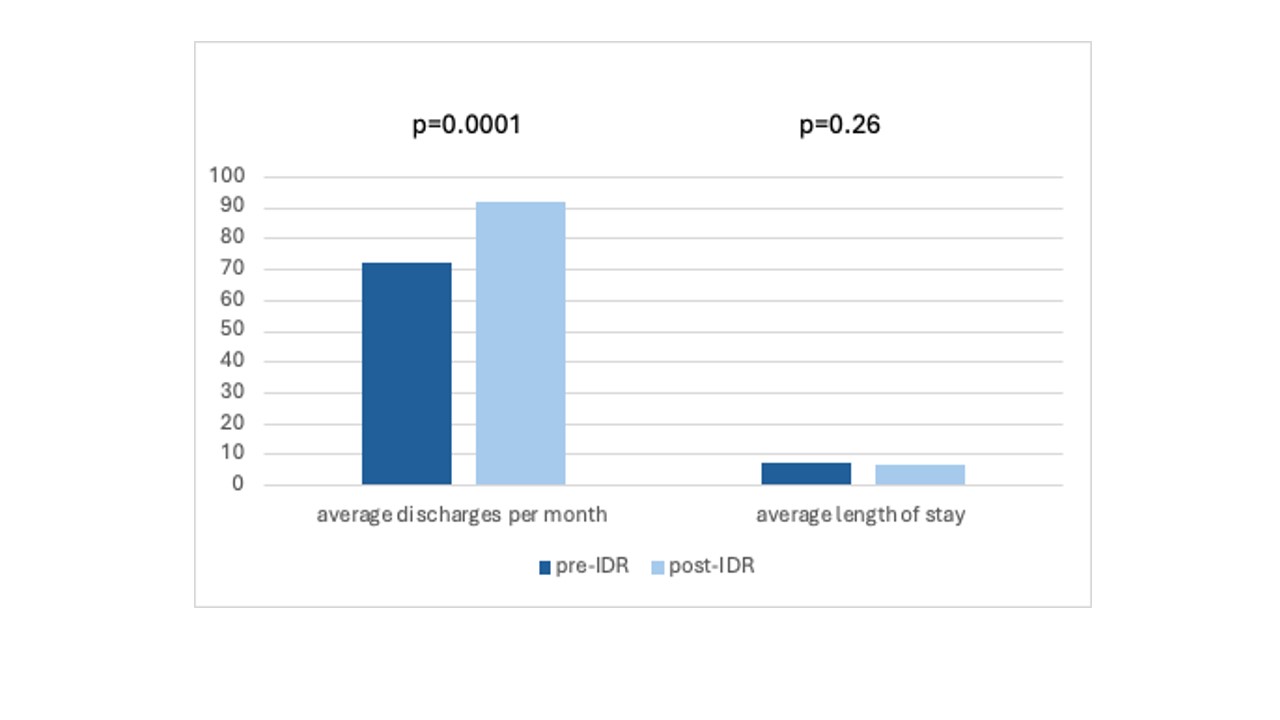
Results: Data shows a statistically significant improvement in the average discharges per month since interdisciplinary rounds initiation (92 vs 72; p .0001). Though length of stay slightly improved this was not statistically significant (7.1 to 7.3; p .26).
Conclusions: This pilot demonstrates that geographic-based rounding and interdisciplinary huddle contributed to a statistically significant increase in average discharges per month. Though length of stay improved, this was not statistically significant. We will continue to collect data on unit 72 to assess for improvement. We will also collect data on additional floors as we expand geographic rounding at EUHM.