Background: Research suggests that high workloads in the inpatient setting (often measured through patient encounters/visits) contribute to increased hospital length of stay, increased costs, and delayed discharges. High workloads also negatively impact our quality improvement efforts and result in a mismatch in job demands and job resources leading to clinician burnout. To date, there is no standardized way to measure total hospitalist work and there are no standards for what an optimal workload is to drive hospitalist, patient, and institutional outcomes.
Purpose: We hypothesize that by developing measures to accurately assess hospitalist workload and the outcomes it drives, we can determine frameworks for safe work standards that improve hospitalist wellbeing, patient care, and operational and financial metrics. We aim to develop an evidence-based approach to building hospitalist staffing models that incorporates clinician data (objective and subjective measures) and electronic clinical data (operational and patient outcomes) to develop a workforce application and safety management platform that drives improved hospitalist, patient, and institutional outcomes.
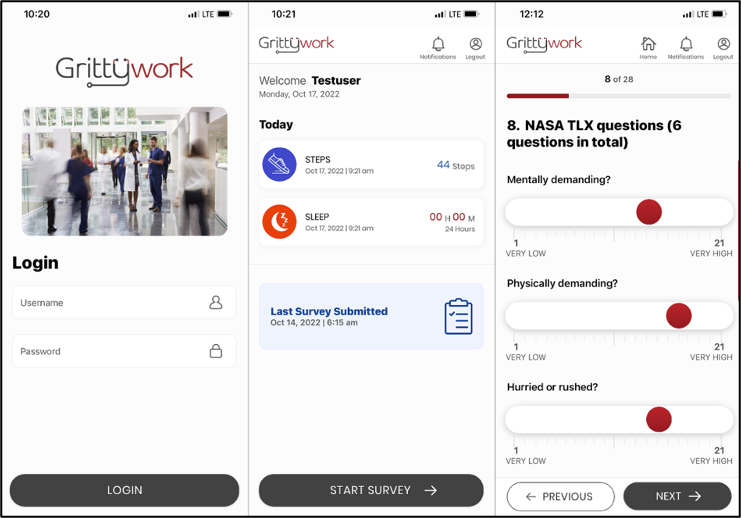
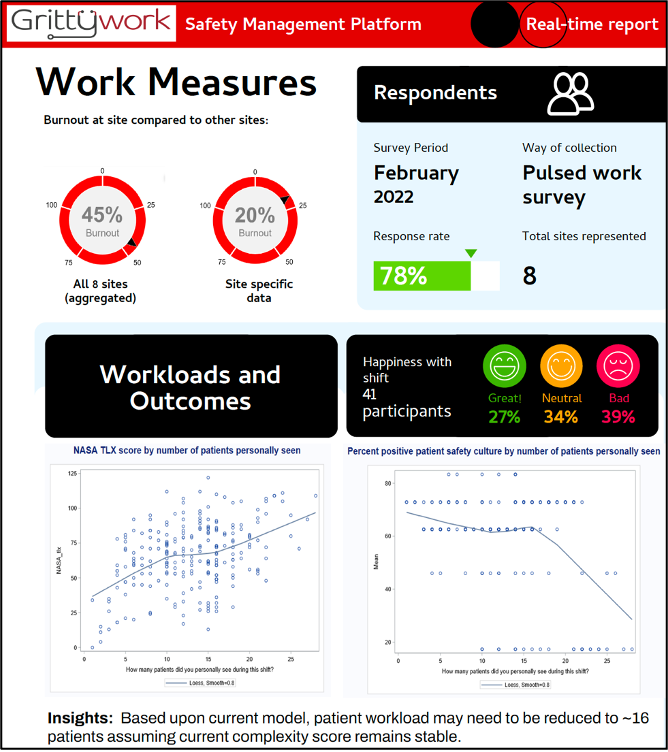
Description: We are taking a multiple methods approach to (1) identify and establish methods to measure total work and (2) develop an intuitive, accessible mobile application and platform with decision support to capture, in real-time, measures of hospitalist workload and pair this with electronic clinical data. The end product will be a safety management platform that offers decision support for hospitalist and hospital leaders to inform data driven and evidence-based staffing practices. To date, we have conducted a Delphi panel consisting of 17 experts from around the country including frontline hospitalists, hospital leaders, administrators, and experts from fields such as human factors engineering and quality improvement. We are conducting a scoping review to identify how workload has historically been defined and measured to better understand its impact on the workforce, patients, and institutional outcomes. Utilizing the measures determined from the Delphi panel and preliminary findings from the ongoing scoping review, we have developed the GrittyWork mobile application (GW app) to measure total hospitalist work. The GW app collects hospitalist perception of work through targeted surveys as well as physical activity data. To guide the design of the tool, we applied the Chokshi and Mann Process Model for User-Centered Digital Development, iteratively modifying the GW app (Figure). We next plan to collect user experience data, specifically using the System Usability Scale (a scale that is industry standard to evaluate satisfaction with a given tool) and usage data (usability and adoption). We will assess the quality of data collected by the mobile application, including the completeness, correctness, concordance, plausibility, and currency of data. Next steps will be to further optimize the tool in preparation for a larger scale multi-site study and to develop a safety management platform that integrates data inputs from clinicians and electronic clinical data to provide decision support to hospital and hospitalist leaders to drive optimal staffing and optimal outcomes.
Conclusions: GrittyWork represents a novel approach to building evidence-based staffing practices to transform hospitalist work and improved hospitalist, patient, and institutional outcomes.