Background: Minority and low-income populations are more likely to be hospitalized and/or re-hospitalized for acute asthma, a key indicator of poorly controlled disease. While hospitals have attempted to improve asthma care by implementing individual-level care interventions, inequities persist during inpatient stays and in intervention delivery. Little is known about the impact of “bundled” systems-level interventions on disparities in asthma care delivery. We conducted an analysis of one such bundled intervention to examine the impact on disparities in implementation.
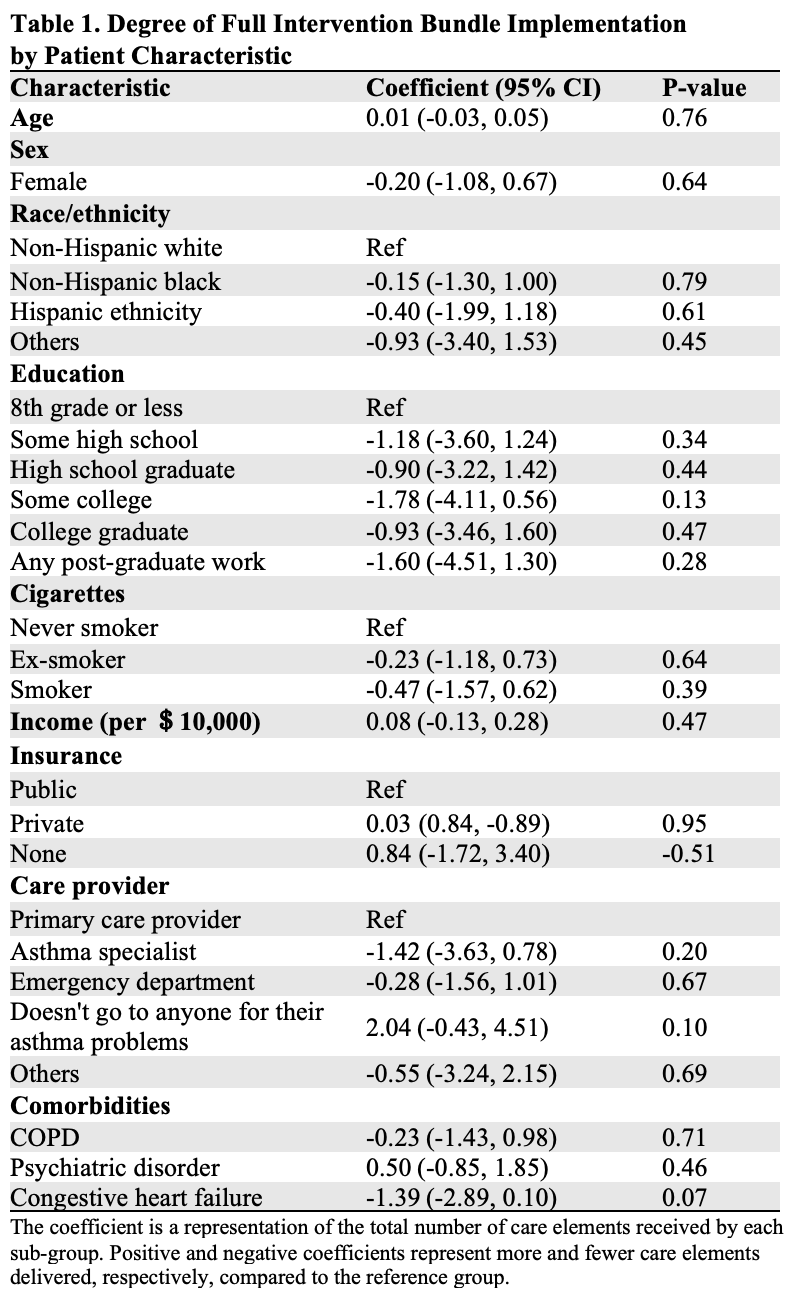
Methods: This is an analysis of data from a prospective multicenter interventional study that enrolled adults aged 18-54 years hospitalized with a physician-diagnosis of acute asthma. The intervention consisted of: 1) laboratory testing, 2) asthma education, and 3) transitional care. A composite concordance score represented patient-level bundle implementation: one bundle item was equal to one point towards each individual’s implementation concordance score (range 0–10). Relationships between patient-level characteristics and implementation of the intervention were examined with generalized linear mixed model regression. Patient-level characteristics included age, sex, race/ethnicity, education, smoking status, socioeconomic status, insurance type, primary care provider, and comorbidities. Associations between patient-level characteristics and implementation of three bundle elements (asthma action plan, inhaler technique education, and follow-up appointment post-discharge) were also studied. Positive and negative coefficients represent more and fewer care elements delivered, respectively (versus reference).
Results: Of 100 adults included in this analysis, the median age was 40 years, 72% were female, 66% identified as non-Hispanic Black, and 12% identified as Hispanic. The median bundle implementation composite score was 6.30 (IQR [5.00-7.60]); no significant differences in overall bundle implementation were found across patient characteristics nor in implementation of three individual bundle elements. In the context of the current study, Non-Hispanic Black and Hispanic individuals were as likely to receive an asthma action plan (0.85 [95%CI: 0.34, 2.09]; 1.69 [95%CI: 0.50, 5.68], respectively), inhaler education (0.85 [95%CI: 0.31, 2.36; 0.72 [95%CI: 0.17, 2.96], respectively), and have a follow-up appointment scheduled post-discharge (0.45 [95%CI: 0.16, 1.31]; 0.49 [95%CI: 0.10, 2.27], respectively) as non-Hispanic White individuals. Further, individuals without insurance coverage (0.84 [95%CI: -1.72, 3.40) received a similar number of intervention care elements as publicly or privately insured individuals (Table 1).
Conclusions: Delivery of a bundled asthma intervention did not differ significantly across patient subgroups. Our findings suggest that a standardized, systems-level, bundle of recommended asthma care elements may decrease the influence of individual provider bias in care delivery. Systems-level asthma care interventions may be effective to address disparities in care delivery and, thereby, improving asthma outcomes across diverse patient populations.